by Nicholas Loh Chieh and Kenneth Lyen published SMA News Oct 2023 Vol 55 pages 20-22



Raffles Hall Musical 4 November 2023

Reviewed by Kenneth Lyen
I was genuinely moved by the Raffles Hall original musical “Oil”. It is about the morality of cheating the public by selling fake famous paintings, and how this can profoundly affect the relationships between friends and family. The title “Oil” can refer to oil paintings but there are also canny meanings like “grease” and “lubricate”. Oil is highly flammable and once lit, it can burn everything in its path.
“Oil” the musical is produced by Xavier Chong, Qian Yi-An and Valerie Oh, and it is directed by Mohammad Afiq Ihsan, Sherise Tan and Teo Tze Yang. The brilliant script is written by Victoria Wong and Goh Zhen Kang, and contains laugh-out-loud humour as well as heart-wrenching scenes. The 10 songs are written by 13 composers, and the music directed by Tan Jun Kiat, the head of music is Ea Hao Wei, and the choral director is Wong Jun Ho. The choreographers Bernice Lee Xin Yi, Ye Huaguan and Ryann Lim created electrifying dance moves and the dancers lifts the scenes with their dynamism.
Based on an art gallery that cheated buyers by selling them fake paintings, it delves into the shady dealings of a husband and wife duo that owns this art gallery but when their illegal dealings were about to be exposed, they placed all the blame on their co-conspirator art forger so they can get off scott free. Unfortunately the art forger dies in prison. His daughter Vesuvia decides to take revenge on the art gallery family that caused the death of her father, by becoming an art forger herself and selling her counterfeit paintings back to these gallery owners. Vesuvia is played by Srividya and she steals the show through her magnificent singing voice and acting. Her mother Bernice is played by Alicia Foo and they have several emotional scenes with each other. Vesuvia’s childhood friend is Amber, played by Clare Madeline, who is unaware of the illicit business of her parents; her father Max is played by Lau Heng Yi and her mother Cecilia is played by Lumiere Chew. The clever investigator who uncovers the shady dealings is played by Nigel Teo, who also steals the show through his convulsive humour.
There is a humorous scene where the gallery owner Max is auctioning a painting by Kazimir Malevich (1879-1935) of a famous black square. Bids are made over $80 millions: incredibly absurd but based on real life. Unfortunately the investigator and his team are at the auction ready to pounce on the art gallery duo owners, and they are arrested. Their daughter Amber is shocked because she has been totally ignorant of her parents’ misdeeds. When she discovers that her friend Vesuvia was the one responsible for her parents’ arrest, she becomes even more devastated. The investigator finds out that Vesuvia was the art forger and goes to arrest her. But her mother protects Vesuvia by falselsy confessing that she is the art forger, thereby taking her daughter’s place in the arrest. Later, when Amber meets up with Vesuvia they quarrel and they break up their friendship.
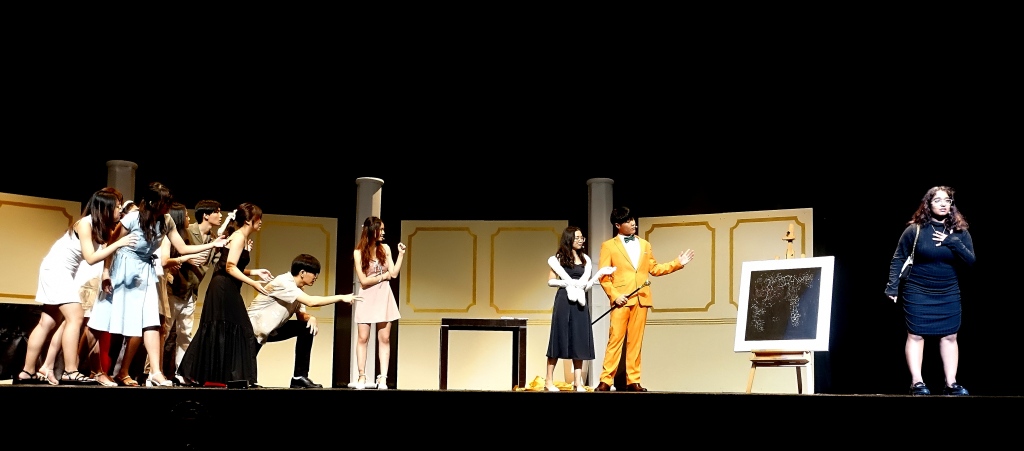
In the end Vesuvia admits that she is the art forger, thus releasing her mother from prison. After serving their sentence, the husband and wife art gallery owners are also released. The reunions of the mother Bernice and daughter Vesuvia, and the parents Max and Cecilia with their daughter Amber are very emotional. The art gallery owner Max tells Vesuvia that since she is incredibly gifted, she should no longer do any more forgery, but devote her artistic talents by creating her own original paintings, and that their art gallery will support her fully. The finale song and dance is an emotional celebration showing that honesty and friendship are more important in life than making money illegally.
Raffles Hall should be congratulated for promoting this musical that espouses principled ethics in a way that touches one deeply. We applaud the JCRC President Lim Choon Wei and the Vice-President Xavier Thng. The Raffles Hall Musical advisor Nguyen Tri Tin spent an enormous amount of time helping every aspect of the musical and his involvement is invaluable. Last but not least, kudos for the success of the Raffles Hall musical “Oil”, must go to the Hall Master, A/Professor Stella Tan. It should go on record that without the Hall Master’s strong involvement and total commitment, there would be no musical.
Congratulations!
Kenneth Lyen
4 November 2023

by Kenneth Lyen
Definition
Bilingualism is the ability to communicate proficiently in more than one language. Skills involved include the ability to listen, comprehend, speak, read, and write in a language other than the mother tongue.
Singapore’s Multilingualism
With a few exceptions, the majority of the world’s countries are actually multilingual, and the citizens can speak two or more languages. Singapore boasts of having four official national languages: English, Mandarin Chinese, Malay and Tamil. Unlike other countries’ multilingualism, Singapore’s four official languages are most divergent, because they do not share any recent common evolutionary ancestry. It is often argued that Singaporeans are actually trilingual because many households speak a separate Chinese dialect such as Hokkien, or a different regional Indian language such as Hindi, which is quite unlike the official national languages of Mandarin and Tamil. Over recent decades, English has gained the upper hand, but bilingualism is still prevalent.
Subtypes of Bilingualism
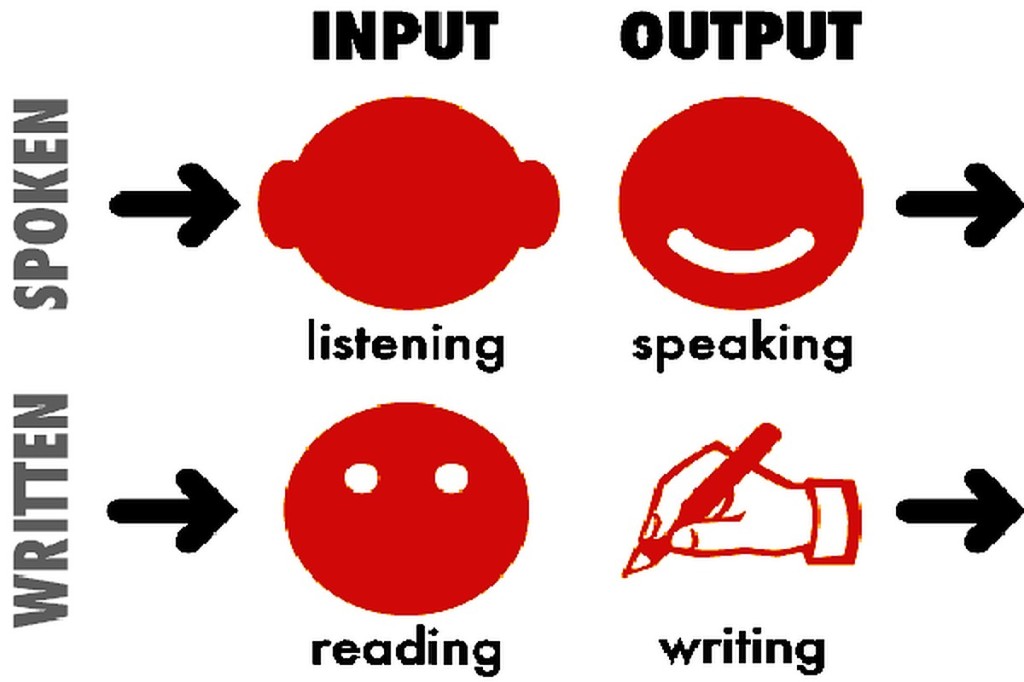
Fundamentally, the brain tackles language in four ways. The initial input is listening, which is followed by the output of speaking. Then later, the input is reading, and the output is writing.
The age at which someone starts to learn a second language can make a difference in the outcome. For example, let’s take a hypothetical family of four who has immigrated to Singapore from a country where they speak a different language, and do not speak any of the four national languages. The family comprises a 3-year old daughter, an 11-year old son, and the parents. There are three subsets of bilingualism which are classified as follows:
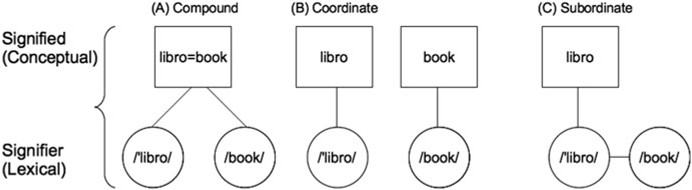
a) Compound
The three-year-old has been learning the native language of the parents, and in Singapore, she attends a preschool and is immersed in English. She readily picks up the second language and begins to process the world around her in this language. Her command of English is excellent, and she might even develop a Singlish accent. As time passes, one language might become more dominant. This should not be seen as a problem because there are many benefits in bilingualism (see below). This early childhood form of bilingualism is known as “compound”.
b) Coordinate
The teenage brother speaks his native language, but in Singapore, he has to learn English from scratch, but fortunately he picks it up very quickly. At school he would speak English to his schoolmates, but at home, he might continue conversing in his native tongue. Over the years, he might speak English predominantly. His bilingualism is referred to as “coordinate”.
c) Subordinate
The parents are learning a secondary language but filters it through their primary native language. They sometimes have to think for a brief moment in order to understand what is said, or translate into English to express their thoughts. They may even have a trace of an accent related to their native tongue. This form of bilingualism is known as “subordinate”.
Because many bilingual individuals can become quite proficient in the new language, and barely colour the speech with their native accents or pronunciations, the difference in their speaking may not even be apparent to a casual observer.
The Brain
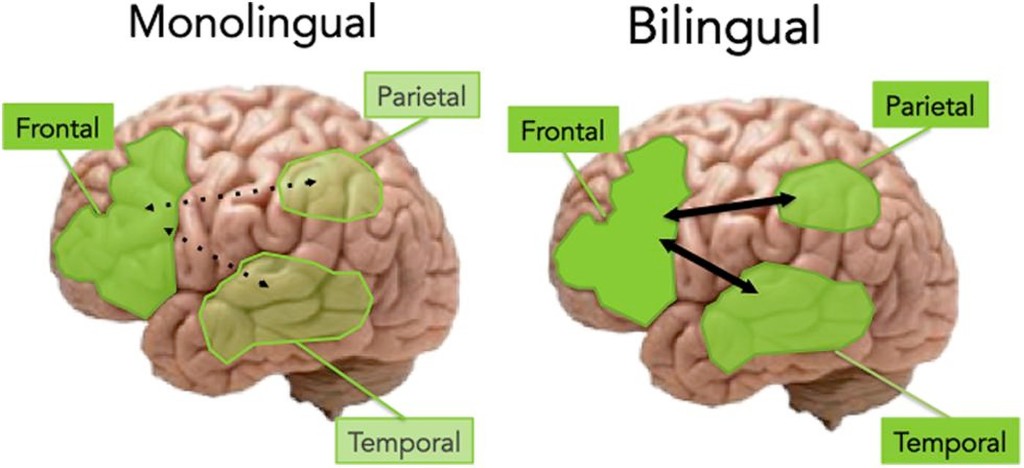
How does the brain handle bilingualism? Functional magnetic resonance imaging (fMRI) and positron emission tomographic (PET) scans have shown increased connectivity between the frontal and posterior parts of the brain compared with monolingual people. This means there is enhanced brain activity as well as improved cognitive reserve.
In early childhood, the brain is more malleable than an adult’s and this plasticity allows the developing brain to use both hemispheres in language acquisition. There is increased density of grey matter as well as more activity between the frontal, parietal and temporal lobe areas when engaging in a second language. In contrast, the adult’s brain development when learning a second language is largely lateralised to the left hemisphere.
The increased activity in a bilingual brain over the years has also been shown to delay dementia, including Alzheimer Disease, by as much as 5 years.
Creole or Pidgin Language

In countries where more languages are spoken, there is a tendency for the speaker to combine two or more languages. This is referred to as creole or pidgin language. This has been classified into 3 degrees of severity:
a) Acrolect: where there is no significant difference between the spoken language from its origins, so listeners have no difficulty understanding.
b) Mesolect: where there are several loan words, plus some dropping of indefinite articles and plural markings on some nouns. Examples of mesolect include “sabo” = “sabotage”, “shiok” = “great” (from the Malay)
c) Basilect: where the combination of words from two or more languages is so severe that foreign listeners have difficulty understanding what is spoken. This is referred to as heavy creole or heavy pidgin. An example is “I buay tahan he talk cock” = “I cannot tolerate his talking nonsense”.
Many speakers of heavy creole or heavy pidgin languages have the ability to switch from this severe form of slang to acrolect or even to the pure speech of the language of origin.
Benefits of Bilingualism
There are many benefits of learning several languages, especially at a very young age. This is backed up by scientific studies, and the bonuses include:

Bilingualism is a national policy in Singapore schools, and is therefore compulsory. However, it has come under some criticisms. The problem is that not everyone is good at learning a second language, and some struggle painfully, and suffer. Another problem is that those who are good at learning languages are not encouraged to learn a third language, such as Malay, Korean, Japanese, or an Indian or European language. Learning extra languages can enhance future careers and business entrepreneurship.
Will Modern Technology Discourage Learning Another Language?
Currently there are many devices that can automatically translate spoken words from one language to another. This means that there is no need to learn a foreign language. It is claimed that even culture-specific swear words, jargon, and slang are all translatable. So the question one will ask is: “Why bother learning another language?” The answer is that present-day devices may not be so good in translating the underlying emotions that accompany one’s speech. Subtle subtext can be lost. For example when one says something sarcastic like “You think you are very clever?” it might be translated in a neutral way, so that the listener might take it as a compliment!
Conclusions
Bilingualism is an important ability that has many benefits, including enhancing brain function, communicating with a wider range of people, delaying dementia, and promoting overseas business. The younger a second language is introduced to a child, the better the long-term outcomes. Their command of the second language will be better, and they will be more flexible and creative in their thinking. Although bilingualism does not increase one’s intelligence, it does delay Alzheimer Disease. It has been shown that even if one did not have the good fortune to learn a second language in early childhood, there are still benefits learning one later in life. It exercises the brain, and as the saying goes, even “a little exercise can go a long way!”

Afterthought: Is multilingualism declining worldwide?
The evidence is anecdotal, but the impression seems to be that fewer people worldwide are multilingual. English-speaking countries like the USA are not actively promoting the learning of second languages, and classrooms discourage speaking in a non-English tongue. The second generation of emigrants to these countries barely speak the native languages of their parents.
Which languages are the first to die? Sadly, the first languages to die off are “die”-lects (sorry for the weak attempt at a joke)!

References
Wikipedia. Multilingualism.
https://en.wikipedia.org/wiki/Multilingualism
Wikipedia. Neuroscience of multilingualism.
https://en.wikipedia.org/wiki/Neuroscience_of_multilingualism
Goksan S et al. Early childhood bilingualism: effects on brain structure and function.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262573/
Skibba R. How a second language can boost the brain.
https://knowablemagazine.org/article/mind/2018/how-second-language-can-boost-brain
Singh Leher. CNA. The benefits of bilingualism go beyond knowing two languages
https://www.channelnewsasia.com/news/singapore/commentary-bilingualism-mother-tongue-language-benefits-9984098
Best voice translator devices on the market in 2021.
https://gadgets-reviews.com/review/1767-best-voice-translator-devices.html
Written by Kenneth Lyen 31 July 2021, Updated 23 August 2021

by Kenneth Lyen
Introduction
The recent death of a 13-year-old schoolboy allegedly caused by a 16-year-old schoolmate, coupled with the rising rate of suicides, has raised concerns about mental health. The increase in psychological distress in children may be related to the current COVID-19 pandemic. The question is whether we are tackling the problems effectively? If not, why not?

First, let us define what we mean by mental health in children.
Definition (1)
Mental health is the complete well-being of a person, including their emotional, psychological, and social life. This affects how one thinks, feels, and acts. It can determine how one handles stress, interact with others, and make choices.
Child mental health is defined slightly differently from adult mental health; it is more nuanced and multifaceted. In addition to emotional and social aspects of psychological health, there is an additional emphasis on behavioural and cognitive functions. A child has unique developmental milestones and experiences which can affect their mental states and thinking over time. Also they may be less able to express their emotions, or they do so differently, which can be misinterpreted or overlooked. Because children’s mental health is a continuum, stretching from early childhood through adolescence, and going all the way to adulthood, the definition needs to embrace the different emotions and expressions associated with the different stages of life.
Presentation (2,3)
It is often said that children wear their hearts on their sleeves. Certainly, younger children may not be able to hide their feelings very well. Late teenagers’ thinking resemble more like that of an adult’s. It is therefore a challenge for parents and teachers to learn how to decipher a child’s behaviour and figure out their underlying meanings.
Changes in behaviour are still the best clues in assessing mental disorders. If a very outgoing sociable young child suddenly becomes reclusive, refuses to eat, does not want to go to school, or refuses to do what they normally do, then something may be wrong. If they are normally close to their parents and then undergo a massive change in behaviour by becoming inconsistent, or shuns spending time to talk to or hug their loved ones, then it is time to delve a little deeper.
Mental health problems of older children and teenagers may be more difficult to detect because they may look perfectly healthy at first glance, until you look more closely their facial expressions or body language. There are certain societal norms that when crossed, may provide clues to potential behavioural abnormalities. For example, if a child becomes inappropriately happy, sad or angry given the circumstances, this can be a clue. Here is a list of the more common signs and symptoms suggestive of mental health problems:
Prevalence (4)
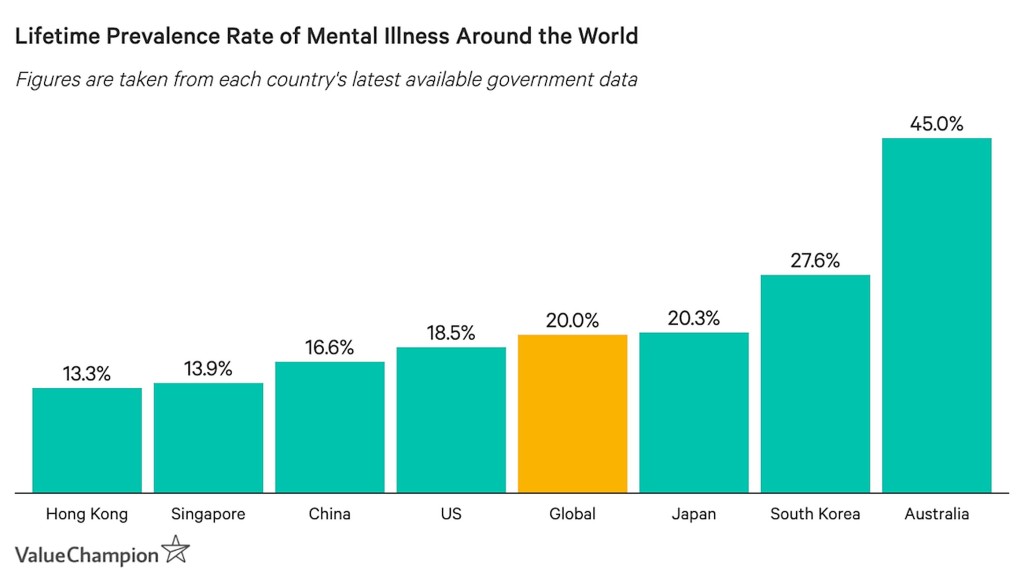
The prevalence of mental health problems in Singapore is around 13.9% which is lower than the global average of 20%, but is nevertheless quite a burden. However, the prevalence has increased during the COVID-19 pandemic.
Psychiatrists have reported an increased number of referrals for mental health issues during the COVID-19 pandemic (5).
Causes
Failing at school tests or exams, scolded by teachers, being bullied at school or cyberbullied on the internet, emotional abuse by friends, can all precipitate mental problems. On top of that, there may be parental conflicts, or other family problems resulting from job losses and reduced financial income. Additional factors include suspension of overseas vacations, limitations of entertainment in cinema and theatre because of reduction in seating capacity, inability to dine out with larger numbers, have added further to mental stress.
Neurodevelopmental Causes
What causes mental health impairments? Twenty-first century science is exploring the answers at a molecular level, where genetics play a crucial role. Brain function seems probably results from an interaction between genes and experiences. This interchange affects mental health, behaviour, personality, and other neurological functions. As to exactly how genes and environment interact to regulate our neurodevelopmental operating systems, remains a mystery.
Physical diseases such as infections, injuries, and side effects of drugs, can certainly affect the developing brain and may lead to longterm behavioural and emotional problems. What is less certain is how emotional stress, poor parental upbringing, and inappropriate school teaching, can destabilize neuronal connections and lead to mental health problems.
Management
One cannot tell if a child has mental health problems just by looking at them. To the outside world they may look perfectly normal. Feeling sad, feeling angry, or feeling stressed out, are all parts of life, just as it is normal to feel happy, confident and carefree sometimes. Positive and negative emotions come and go, depending on what is happening around that person. How does one tell if a child is having significant emotional problems? And if they do have such problems, how does one go about restoring them back to mental health? Here are some steps that practitioners have recommended for both the child as well as the adult:
1 Talk
This is the most important step to take. Talk to your child and listen to their feelings and thoughts without any pressure or judgement. Sometimes overwhelming feelings are brought on by events in one’s life, sometimes they happen for no reason at all, and it may be helpful to talk about these emotions. For adults, if you have direct voice contact with your friend or colleague, you can use this means to share your thoughts. Alternatively, you can communicate with them via social media.
2 Exercise
One of the best tools for treating anxiety and mild depression is physical exercise. Help your child exercise at home, or play indoor or outdoor sports. If the gym is open, you can go there more regularly. Even if you are in a lockdowns or stay-home notice, you can try to get some fresh air on the balcony. But if it is possible, go outdoors for exercise and walks.
3 Take a Break
Take a break and do something your child enjoys: drink a hot drink, watch Netflix, play with a pet, or whatever makes you and your child feel better.
4 Express Your Feelings and Thoughts
Encourage your child to write a journal or a blog, write some poetry, do some art, or music …

… or do some photography, start a Vlog, or dance on TikTok.

5 Volunteer to Help Others
Volunteer for social service: you and your child can help deliver food and groceries to disadvantaged people, give online tuition for the underprivileged, or learn to be a mental health advocate.
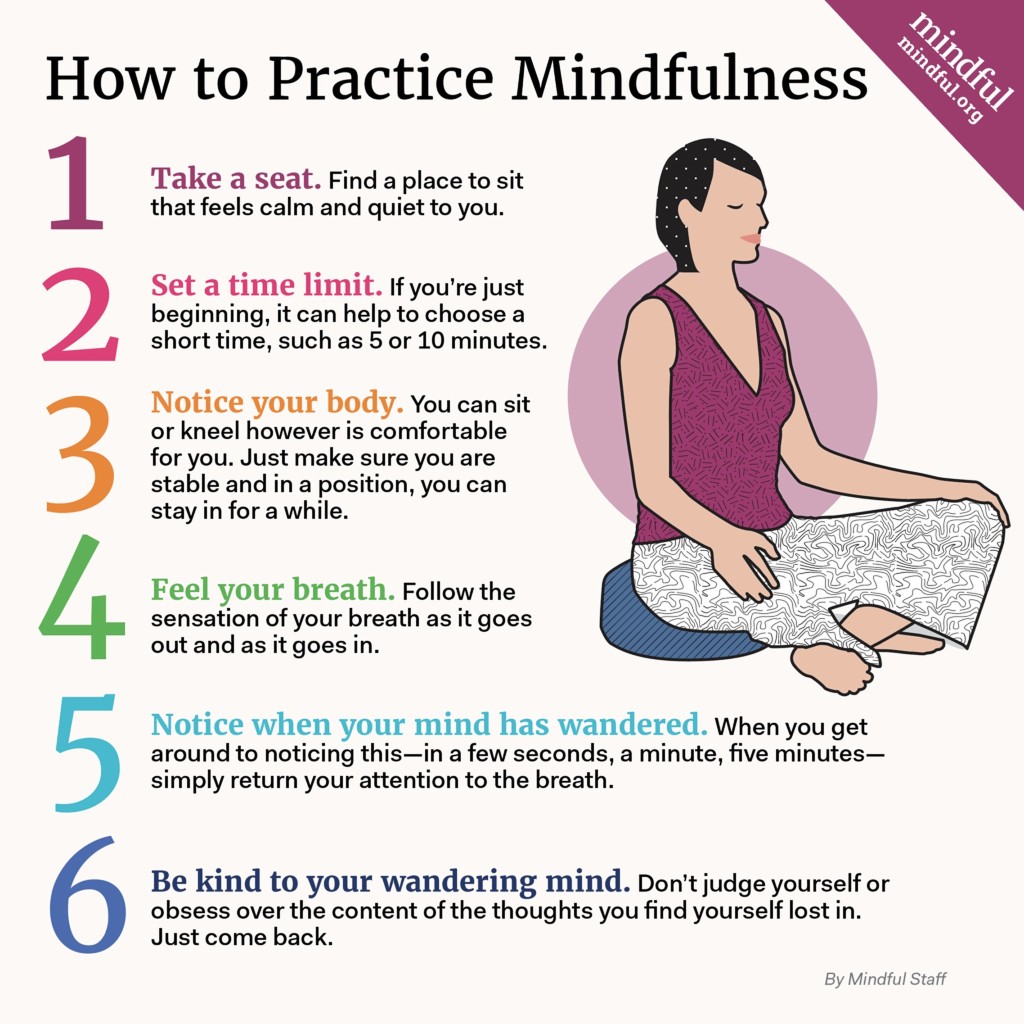
6 Mindfulness
You can practice mindfulness or do some yoga.
7 Consult a Professional
If you or your child is still feeling down, you might consider consulting someone else who might be able to give some professional advice.
8 Limit Access to the Daily News
No news is good news. Currently most of the news on television and newspaper tend to focus on bad news, such as the spread of COVID-19 and the mortality rate. Therefore, it may be advisable to restrict one’s access and time to listen to the news.
Educating Parents, Caregivers and Teachers
The issue of educating caregivers lies at the root of adult emotional literacy. In general, parents are not taught how to be good parents. They are not taught what is the optimal response to their child’s misbehaviours, temper tantrums, and refusals. Asian parents are often viewed as being too strict with their children and they may often resort to caning or physical punishments. They have not been educated on how to display empathy and compassion to a misbehaving child. Many parents discipline their children in the same way that they themselves were disciplined during their own childhood.
How should parents respond to emotional problems or traumatic events? Should they reprimand a crying child and tell them to stop crying, or give them an angry look? Well, this might deter the child from expressing their feelings to their parents, and they will likely repress their emotions. When this scolding recurs over time, the child might react in the form of aggression, rage, or shouting. And then later, this can evolve into bullying behaviour, or even turn up as violence. But if the child is doing something potentially dangerous, then it may be appropriate to shake one’s head and give a stern look.
On the other hand, when parents respond to sadness or crying by saying: “It’s OK for you to express how you are, I will accept all of you, the angry, the sad, as well as the happy bits of you. Let me hold you for a moment.” When you display empathy and compassion to the child, and show that home is a safe place to be, then after they have calmed down, you can explain why you think they should behave in a more rational reasonable way.
However, if the child is crying because you have denied them something they want, then it is important not to capitulate and give them what they want. This would encourage crying as a means to manipulate you, the caregiver to acquiesce to their future demands.
Educating parents, caregivers, and teachers is therefore an important part of child-rearing.
What About The Education System?
The other problem in Singapore and some other countries, is that parents value IQ more than EQ, and some rate exam scores more highly than integrity. Over the years, the educational system has become more rigid, more stressful, more hyper-competitive, and less enjoyable. It is becoming more like an Olympic Games sport that only gives you one chance to prove yourself. It is unforgiving. If you are knocked out in an early round, there is no second chance to allow for a comeback. Many parents send their children for extra tuition in order to gain an advantage in school exams.
No wonder most Singapore school children are frustrated and stressed out. It makes them perpetually anxious and fatigued, and there is little enjoyment in school life. This can lead to further anxiety, sadness, and depression.
Children develop at different rates and some may be better at certain subjects and not others, or some might excel in the arts or in sports. The rather unimaginative exam system, often using multiple choice questions also limits creative thinking and adds more stress to schoolchildren.
Exam stresses are a perennial problem. Children worry that they are falling behind in their revisions. If they did well in a previous exam, then expectations are for them to do as well, if not better, than their last achievements. And when they do badly, it feels like having won an Olympic medal last time, but unable to defend one’s title currently. Then there is the additional pressure of parental expectations. Parents are hovering in the background and even if they do not voice their demands, their child automatically assumes they desire nothing less than coming top of the class. These pressures can be overwhelming, especially for schoolchildren.
The inability for children to physically attend school during periods of pandemic lockdown, the restrictions of going outdoors and being stuck at home, the change in classroom teaching to home-based Zoom learning, has had some adverse emotional impact.
Suicide rates among school children has been high, but recently with COVID-19, there has been an increased spike in cases (7,8). This requires urgent attention. Fortunately Singapore is addressing this problem (9)
Conclusions
Mental health of children, when managed in a sensitive, exemplary way, can lead to a well-balanced, selfless, ethical, humane adult, someone capable of thinking critically and creatively. This requires careful cultivation of appropriate care of children by parents, caregivers, teachers and friends. We recognize that each child is different, and that education needs to be individualized and customized for the different stages of child development. Much more attention must be devoted to this area of child development. Hopefully changes will come soon.
For information about mental health in Singapore, go to the Institute of Mental Health Singapore’s website (10) . You can also read my article on Depression and Suicide (11).
References
1 Wikipedia. Mental health.
https://en.wikipedia.org/wiki/Mental_health
2 American Psychiatric Association. Warning signs of mental illness.
https://www.psychiatry.org/patients-families/warning-signs-of-mental-illness
3 MentalHealth.gov. What is mental health?
https://www.mentalhealth.gov/basics/what-is-mental-health
4 Evlanova A. Yahoo Finance. What is the state of mental health in Singapore?
https://sg.finance.yahoo.com/news/state-mental-health-singapore-192021797.html
5 Ong A. Channel NewsAsia. Worries over COVID-19 situation are taking a mental toll on Singapore
6 Channel NewsAsia. A hyper-competitive culture is breeding severe test anxiety among many students.
7 Straits Times 3 Aug 2020. Youth suicides still a concern, with 94 cases last year and in 2018.
https://www.straitstimes.com/singapore/number-of-suicides-in-2019-did-not-decline-compared-with-2018-youth-suicides-still-a
8 Channel NewsAsia. MOE, MSF ‘very concerned’ about spike in youth suicides; experts say more support and awareness necessary
https://www.channelnewsasia.com/news/singapore/moe-msf-very-concerned-about-spike-in-youth-suicides-experts-say-11775260
9 Straits Times 27 July 2021. MOE to strengthen support networks in schools; all teachers to get enhanced training on mental health literacy
10 Child Guidance Clinic Singapore.
https://www.imh.com.sg/clinical/page.aspx?id=283
11 Lyen K. Depression and Suicide. https://kenlyen.wordpress.com/2021/07/13/depression-and-suicide/
Getting Help
National Care Hotline: 1800-202-6868 (8am to noon)
Mental Well-Being
Mental Health Helpline: 6389-2222 (24 hours)
Samaritans of Singapore: 1800-221-4444 (24 hours)
Singapore Association for Mental Health: 1800-283-7019 (Mon to Fri 9am to 6pm)
Silver Ribbon Singapore: 6386-1928, 6509-0271 (Mon to Fri 9am to 6pm)
Tinkle Friend: 1800-274-4788 (Mon to Fri 2:30 to 5pm)
Counselling
Touchline 1800-377-2252 (Mon to Fri 9am to 6pm)
Care Corner Counselling Centre (Mandarin): 1800-353-5800 (10am to 10pm)
Written by Kenneth Lyen 28 July 2021

by Kenneth Lyen
Introduction
Children follow a familiar timetable for development, a given calendar for achieving motor, communication and social skills. Like the steps of a staircase, one climbs one step at a time.

Most children learn to walk and talk soon after their first birthday. They join two to four words into a phrase by 2 years, copy a circle by 3 years, and count up to 10 around 4 years old. Parents get very worried when their child does not reach these milestones at the expected time, and they might ask around to check if their child is developmentally delayed. They get even more worried when they hear that their child is suspected to be “intellectual disabled”. What does this term mean?
Definition (1,2)
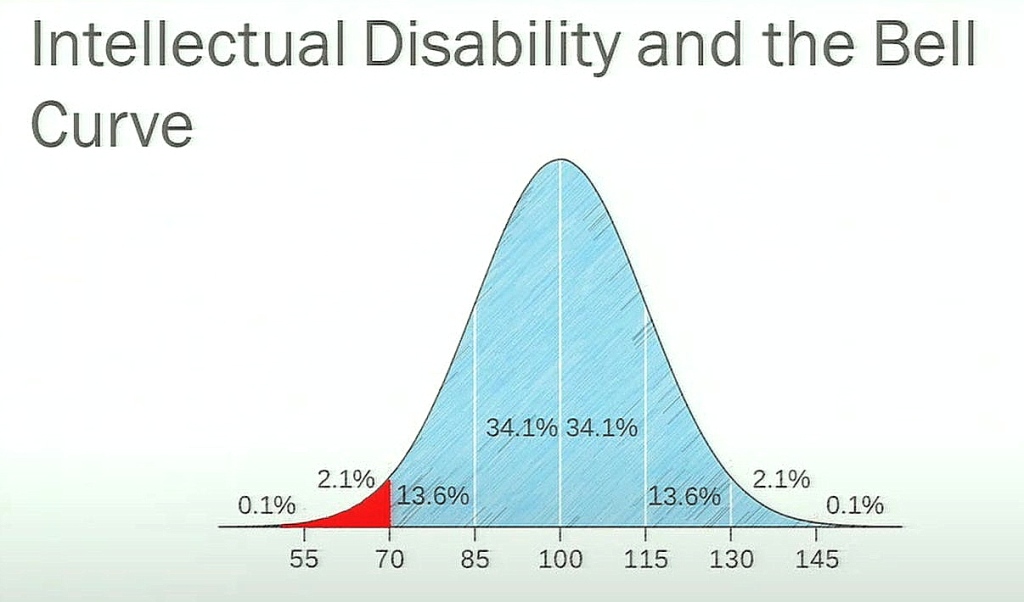
Intellectual disability is an impairment of mental abilities that impacts adaptive functioning, with an onset during a person’s developmental period (<18 years).
The intellectual function is significantly below average when formally tested, and the IQ score is <70. This results in problems with one’s abilities in learning, reasoning, and problem-solving.
Intellectual function can impact adaptive behaviors, and the areas affected are classified as conceptual, social and practical skills:
Ability to handle the concepts of numbers, money, and time
Capability of self-direction so as to live independently
Social responsibility
Self-esteem
Gullibility, naivete
Social problem solving/rules
Occupational skills
Healthcare
Travel and transportation
Use of money and the handphone
IQ Tests
The definition of intellectual disability is based on the IQ test. There are several IQ tests available for children over the age of 1 year (4). However, it is sometimes difficult to decide which test is the best. For children under 2 years old the Bayley Scales for Infant and Toddler Development (Bayley III) is the only one available. For children above the age of 2 year, the Wechsler Intelligence Test for children (WISC) is popular. The oldest test, the Stanford-Binet IQ test is also available and some psychologists are still using it.
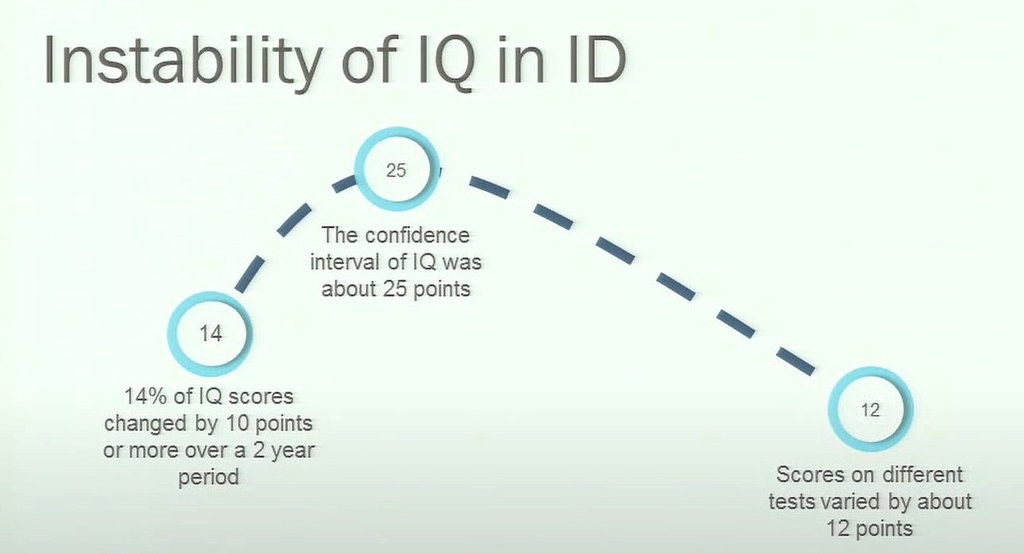
The problem with conducting IQ tests on children is that their cooperation is essential, but this may not be forthcoming. There is an error of plus or minus 5 points using the same test. About 14% of children’s IQ will change by 10 points or more on follow up, over a 2-year period. At the 95% confidence point, several IQ tests report a confidence interval of 25 points, which is rather high. Different IQ tests have shown scores that can vary by 12 points. Hence the inaccuracy and instability of IQ test scores especially when applied to children, makes one wonder about their reliability, and whether a wrong reading can be problematic (5).
Exclusionary Criteria
Factors that can distort IQ testing include the presence of other factors, such as hearing or visual impairment, or if the child has attention deficit hyperactivity disorder (ADHD), or is feeling sleepy, or cannot read clearly because of dyslexia. Therefore, to come to a more accurate diagnosis of intellectual disability one must rule out the following:
Ensure that the IQ test is conducted by an experienced qualified psychologist who has given appropriate instructions understood by the test subject. If the results are unclear, it may be necessary to repeat the assessment.
Levels of Intellectual Disability (ID)
It is traditional to classify the degree of intellectual impairment based on the IQ score, and one then tries to correlate the score with the degree of support the individual might requires in daily life:
Using the level of IQ to match their functioning level is problematic, because it is not an accurate reflection of life skills. Rather than use the IQ score as the basis, it is better look at it the other way round, and base one’s assessment on needs, rather than an inaccurate IQ number:
How Common is Intellectual Disability?
The estimated worldwide prevalence of intellectual disability is between 1-3% of the population (3). How does it compare with other childhood disorders?
Causes
Intellectual disability is thought to be the result of miswiring of the nerves in the central nervous system. This results in slowing down or even stopping nervous signals in their tracks. The brain is our supreme command centre which controls our thoughts, our memories, our speech, the movement of our limbs, and the function of many organs inside our body.
Damage to the developing brain causes miswiring of the nerves, and this can occur before, during, or after birth. We divide the causes into two major categories: genetics and environment. We realise that these two divisions may not be totally isolated from each other, and they can interact with one another. To this day, unfortunately, there are still people with intellectual disabilities where we cannot fathom the cause(s), and they remain a mystery.
Genetic Causes (6)
Genetic causes include chromosomal abnormalities, inborn errors of metabolism and random gene mutations. There are literally hundreds of genetic causes, listed in the given references. The commonest chromosomal abnormality associated with intellectual disability is Down Syndrome. Gene mutations are also found in William Syndrome, Prader-Willi Syndrome, Fragile-X Syndrome, Rett Syndrome, etc.


What is the link between genetics and brain development?
Genes control protein synthesis and all cells, including nerve cells are made of proteins. The function of cells are controlled by enzymes and other proteins. Hence genetic mutations of brain cells can result in abnormal protein production, hence potentially affecting the structure and function of the brain.
a) Brain malformation affecting the structure of the brain
Microcephaly restricts the development of neurons
Macrocephaly
Abnormalities in brain architecture eg Lissencephaly
Agenesis of the corpus callosum
b) Disruptions in cellular metabolism with anomalies in the manufacturing and regulation of molecules essential to the brain and nerves
Insufficient transport of necessary substances inside the cell
Inadequate protein formation (transcription and translation)
Lack of energetic substrates for the cell (mitochondria)
Accumulation of toxic substances
c) Abnormalities affecting the ability of neurons (the main brain cell population transporting information) to connect to each other: brain plasticity
Brain plasticity is essential to acquire new skills through the many connections between neurons as experienced and stimulated by the environment
When cerebral plasticity is impaired, brain functions are restricted, resulting in altered information processing, inappropriate emotions and language difficulties, making it difficult for the person to adapt to the environment
At the same time the brain becomes more excitable and less able to filter information to protect itself from sensory over-stimulation and strong emotions
In addition to intellectual disability other disorders may accompany the intellectual delay:
Language disorders
Learning delays
Emotional control difficulties
Motor disorders
Epilepsy
Behavioral disorders
Sleep disorders
Eating disorders
Genetic defects may not be limited to neuronal cells: other organs may include heart, kidneys, eyes.
Environmental Causes
Problems during pregnancy can affect the developing foetus, including hypoxia, maternal drugs, alcohol abuse, infections, etc. These can cause brain damage leading to intellectual disability.
Postnatal causes: jaundice, infections (meningitis, whooping cough), drowning, accidents, exposure to drugs and chemicals, malnutrition, can affect brain development.
Investigations
A doctor needs to take a full medical history and do a physical examination including doing a thorough neurological examination, and looking for signs of hypothyroidism. The height, weight, head circumference and blood pressure must be measured.
Laboratory tests should include thyroid function, vitamin D level, full blood count, tests for congenital infections, and chromosome studies.
Magnetic resonance imaging or computed tomographic scan, and skeletal Xrays may be necessary.
Therapy
Currently, there is no cure for intellectual disability, at least not yet. We are able to help these children achieve their maximum potential through special education and several intervention therapies, including speech therapy, occupational therapy, physiotherapy, music and art therapy. Should the individual display other disorders, such as epilepsy, ADHD, depression, sleep disturbances, etc, they should be treated if and when these symptoms arise.
Gene and CRISPR Therapy
Some gene mutations can lead to the production of abnormal proteins which might cause disruptions of nerve connections. If this were the case, then can we replace the defective or missing gene(s)? The answer is not at this moment. But looking at the successful introduction of gene therapy for other genetic diseases like haemophilia, severe combined immunodeficiency and retinitis pigmentosa, and CRISPR technology for sickle cell anaemia (9), it will not be long before gene therapy might become available for neurodevelopmental conditions.
Dietary Therapy
It has been observed that deficiency of vitamin D, vitamin B12, folic acid, iodine, and severe iron deficiency is associated with impaired intellectual function. Mental activity improves when these deficiencies are corrected. We are already treating metabolic diseases like phenylketonuria and galactosaemia by avoiding phenylalanine and/or milk. Other dietary manipulations that have shown benefits, include a ketogenic diet rich in fat plus non-synthesized vitamins such as biotin or thiamine, or by providing a missing enzyme with enzyme therapy.
Tuberose Sclerosis
Tuberose sclerosis is an autosomal dominant disorder causing intellectual disability and severe epilepsy. The mTOR molecular pathway becomes hyperactive when stimulated by the hamartin protein manufactured by the defective genes. A new drug, everolimus has been approved by the US Food and Drug Administration for use in tuberose sclerosis (7).
Fragile-X Syndrome
Fragile-X Syndrome is inherited as an X-linked dominant. It causes a disruption of the GABA and glutamate molecular pathways, resulting in interrupted neuronal communications which leads to intellectual disability and epilepsy. Sertraline, a selective serotonin reuptake inhibitor, has been shown to be helpful in reducing some of the symptoms of this syndrome (8).
Special Education
Early Intervention

Early diagnosis and intervention though special education and behaviour therapy has been shown to maximize the child’s potential. The class size should be kept as small as possible so that the teacher-student ratio is kept low. The training and therapy is best conducted by specially trained teachers and therapists. The curriculum is holistic and inclusive, and the pace of teaching is individualized, depending on the rate at which the child progresses.
The areas covered in the early intervention program include:
a) Cognitive domain: learning language, both verbal and written, handling numbers, mathematics calculations, problem-solving.
b) Social and communication skills: This is conducted through direct interaction with the therapists and the student peers.
c) Arts, music, sports: Students learn how to sing, dance, play a musical instrument, they are taught drawing and painting, and play several sports including swimming.

d) Behaviour guidance: if the child’s behaviour is challenging (eg too aggressive or too passive), gentle modification is introduced.
For more details regarding referral to Early Intervention and Special Education in Singapore please see the reference below (10).
Continuing Education
In Singapore, there is a trend for the mildly intellectually disabled children to be integrated into regular mainstream nurseries, kindergartens and primary schools. The more severely disabled are still segregated into separate schools. Most special schools take children up to the age of 18 years. Sheltered workshop and training for outside employment for those above 18 years is still limited.
Helping the Family
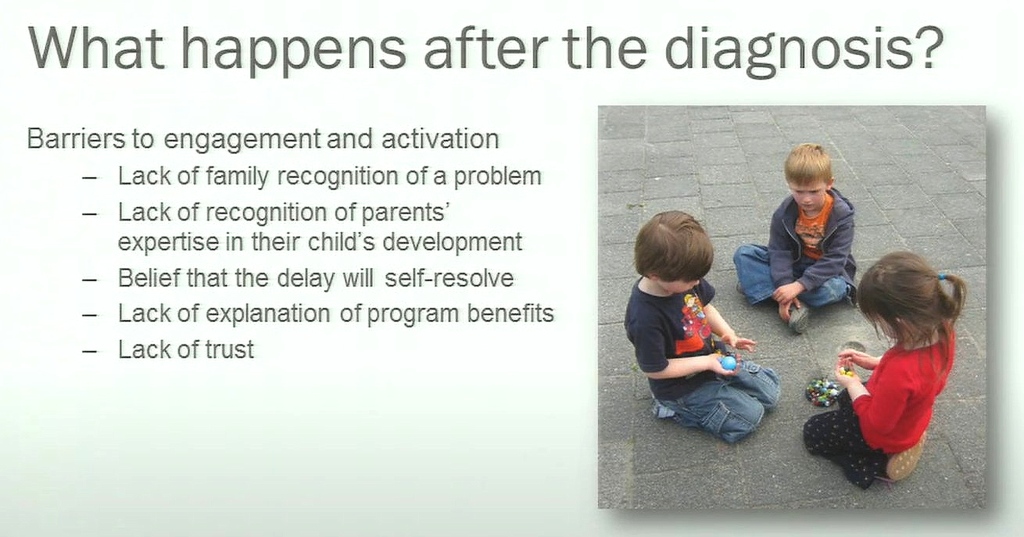
When parents are informed by the doctor that their child could be intellectually disabled, they may take the news badly, and either disbelieve the information, or become depressed. It is important for the doctor to be prepared for either response, and if the parents might like to have a relative or friend also to be present when the diagnosis is being presented. It is important for the doctor to spend time to listen to what the parents feel, and if the do not believe the news, then either have someone else also talk to them, or invite them back for another consultation. The parents may want to seek a second opinion, and the doctor should be able to recommend someone else. The doctor might take a neutral or slightly optimistic long-term forecast on how the child can improve with early intervention and treatment. It is best to give the family some hope.
Conclusions
Intellectually challenged children are declining in numbers, thanks to preventive measures like rubella and other vaccinations, and better antenatal and birth management. Gene and CRISPR therapy is starting to show some promise, but they are not readily available for the time being. Medicines can be used to treat some of the associated conditions, such as epilepsy, ADHD and depression. The backbone of therapy for these exceptional children is education supplemented by speech and other therapies. Intervention should be introduced as early as possible to maximise the child’s potential. It is hoped that in future these children can become more fully integrated into the mainstream educational system. We should treat them as part of our family, and take care of them from birth to departure as family members.

References
1 Wikipedia. Intellectual disability https://en.wikipedia.org/wiki/Intellectual_disability
2 eMedicine. Inrellectual disability https://emedicine.medscape.com/article/1180709-overview#showall
3 Special Olympics. Worldwide prevalence of intellectual disability. https://www.specialolympics.org/about/intellectual-disabilities/what-is-intellectual-disability
4 Chow A. Psychometric & IQ testing. https://www.annabellepsychology.com/iq-testing
5 Oxford Learning. What’s the score? Problems with IQ tests for kids. https://www.oxfordlearning.com/whats-the-score-problems-with-iq-tests-for-kids/
6 Llyas M. The genetics of intellectual disability: advancing technology and gene editing https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6966773/
7 FDA approves everolimus for tuberous sclerosis complex-associated partial-onset seizures https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-everolimus-tuberous-sclerosis-complex-associated-partial-onset-seizures
8 Science Daily. Sertraline improves functioning in young children with fragile X https://www.sciencedaily.com/releases/2016/08/160826151740.htm
9 Thomas I. CNBC: CRISPR gene-editing treatment can reach patients very very soon. https://www.cnbc.com/2021/07/02/crispr-gene-editing-could-reach-patients-very-soon-intellia-ceo.html
10 Singapore Ministry of Social and Family Development: referral for Early Intervention and Special Education https://www.msf.gov.sg/policies/Disabilities-and-Special-Needs/Enabling-Masterplans/Pages/Early-Years-Ages-0-6.aspx
Written by Kenneth Lyen, founder of the Rainbow Centre 26 July 2021
by Kenneth Lyen
Introduction
“I brought my 6-year-old son to see you because his teacher says he has attention deficit hyperactivity disorder (ADHD)”, an anxious mother told me. “He cannot sit still, keeps on interrupting the teacher by asking endless questions, and does not pay attention, reading books all the time.” I asked mother what her son was particularly interested in, and the boy immediately barged in saying he was interested in the ice tundra, astronomy, dinosaurs, and Harry Potter books. All the while, he was fidgeting in his chair, twirling round and round. His mother told him that despite getting bad reports from the teachers, he always did well in mathematics and other tests.
I referred him for formal psychological testing and the report said that this boy did not have ADHD, but rather he had gifted intelligence. His behaviour was overactive, not hyperactive, probably because he was able to learn things very quickly, and got bored in class when lessons dragged on at a snail’s pace.
Definitions
There are many adjectives we use to describe intelligent people, such as “clever”, “smart”, “bright”, “brainy”, scholarly. Some intelligent people are especially talented in certain areas, like mathematics, language, music, art and sports. Does that mean there are many types of intelligences? And what is the relationship between giftedness and intelligence? And how does giftedness differ from talent? First, let us try to define these concepts.
Intelligence
Intelligence can be defined as a general mental aptitude that involves several capabilities, including the abilities to reason, to solve problems, to think abstractly, plan ahead, learn from experience, understand and memorize complex ideas.
Intelligence can be measured by an IQ test. However, this is limited to mathematics, visuospatial and language measurements, but it appears that there appears to be a general factor (g factor) which crosses into other assessments of intelligence (see below for IQ tests).
Giftedness
Giftedness is a quality or attribute where a person displays exceptionally high achievement capabilities in areas of intellectual, creative, artistic, leadership capacity, or in specific academic fields.
Children may be born with the potential of developing giftedness. In other words, there is a gifted genetic seed which can grow and flourish best when given the right nourishing environment.
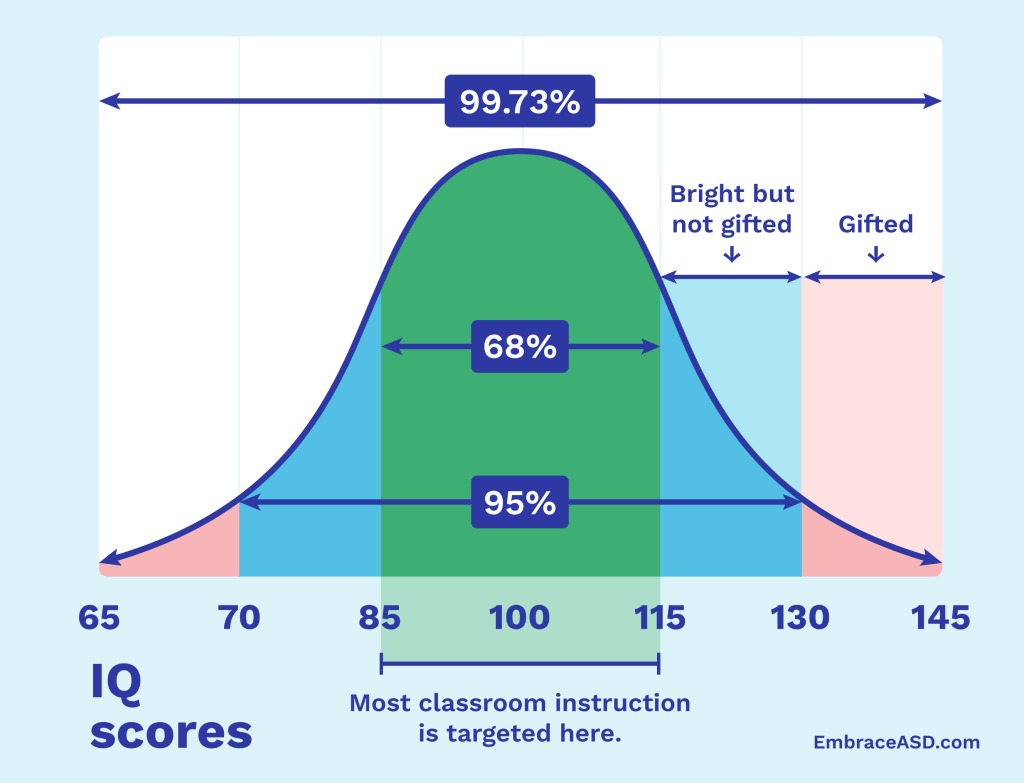
Giftedness is usually linked to a high intelligence, with an IQ of 130 or higher, which is found in the top 2% of the general population.
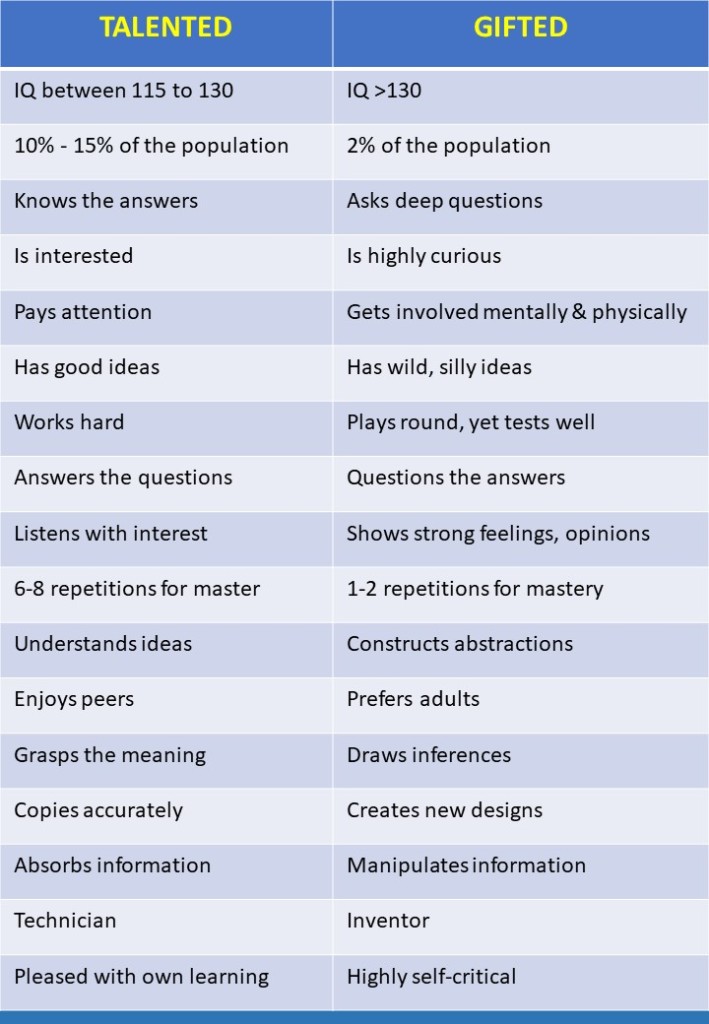
Talented
To be talented is to have the natural ability or skill to do something very well. Often the areas of ability are in the arts, sports, and school performance.
Gifted vs Talented
The major differences are that gifted people display outstanding natural abilities and exceptional talents. There are far fewer gifted people in the general population. Talented individuals are also very skillful and have brilliant abilities in many areas including dance, music, design, sports, writing, and arts. Gifted people tend to think differently, and are more driven. However, there is some overlap between gifted and talented persons. Major differences are outline in the table below:
IQ Tests and the Labeling of Giftedness
Despite the limitations, the most objective tests for diagnosing giftedness is the IQ intelligence test. The Stanford-Binet test was developed by Lewis Terman, the professor of psychology at Stanford University, in 1917. It was modified from the original Binet-Simon test (1905), and remains the foundation of current IQ tests.
Since then, there have been many more IQ tests developed. For children, the most popular is the Wechsler Intelligence Scale for Children.
For entry into many educational programs, the IQ test forms an important component of the entrance exams. For example, entry into the Singapore secondary schools requires students to sit for the Primary School Leaving Exam (PSLE). For university entry, the US universities have a Scholastic Assessment Test (SAT), the British medical schools’ tests include the University Clinical Aptitude Test (UCAT), the BioMedical Admissions Test (BMAT), and for international students applying to Australian medical schools, they have to take the International Student Admissions Test (ISAT). A major component of all these exams is the IQ test.
Gifted Education

It has long been recognised that some gifted children have difficulties negotiating the conventional educational system. Their minds are racing ahead, but they are dragged back by their slower classmates. Therefore, many countries offer education for gifted children on a voluntary basis.
In order to be admitted into such a program, children have to take a special exam, which includes an IQ test.
In Singapore, the top 1% of that year’s cohort are admitted to the gifted program. IQ forms the major component of the selection criteria. Although the actual IQ might fluctuate from year to year, in general the gifted program selects children whose IQ are greater than around 140. The test is taken when the child is 9-10 years old.
There has been a lot of debate concerning gifted education. The first is the use of IQ tests for admission into the program. Below are listed the pros and cons of using IQ tests to select students:
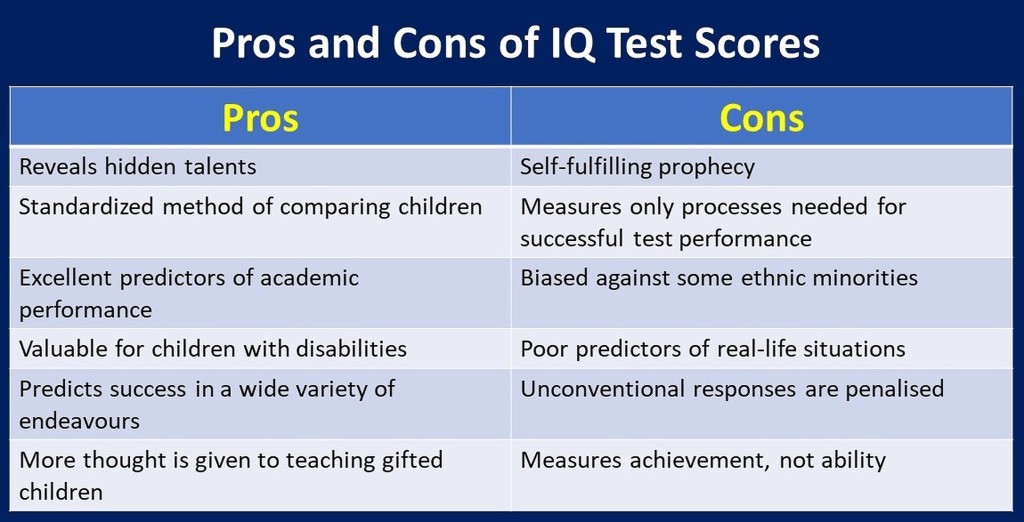
Interviewing children and parents who have been through gifted educational programs, the general consensus is that the benefits of the gifted education system outweigh the risks of remaining in a regular mixed ability class. Most children enjoy the program, they like to mix with children of similar intellect, they love being taught by better teachers, being stretched academically, and covering the curriculum at a greater depth. The majority of these gifted children continue to do well right through university and their chosen future professions.
One of the recurring objections to the gifted education program is that it creates a class of elites. One teenager in the gifted education program was asked if she knew a child attending a normal class in her school, and she answered: “I do not mix with normal students”! To minimise this concern of superiority and elitism, many gifted education programs try their best to integrate the children of all abilities to participate together in non-academic areas including art, music, drama, sports, and community service.
Some critics say that not all gifted children remain gifted throughout their lives. This criticism has been tackled by allowing free flow of gifted children in and out of the program. Singapore only accepts children in the top 1% of the population into the gifted program, and both the child and the parents must accept the opportunity being offered; thus reducing the possibility of making wrong admission choices.
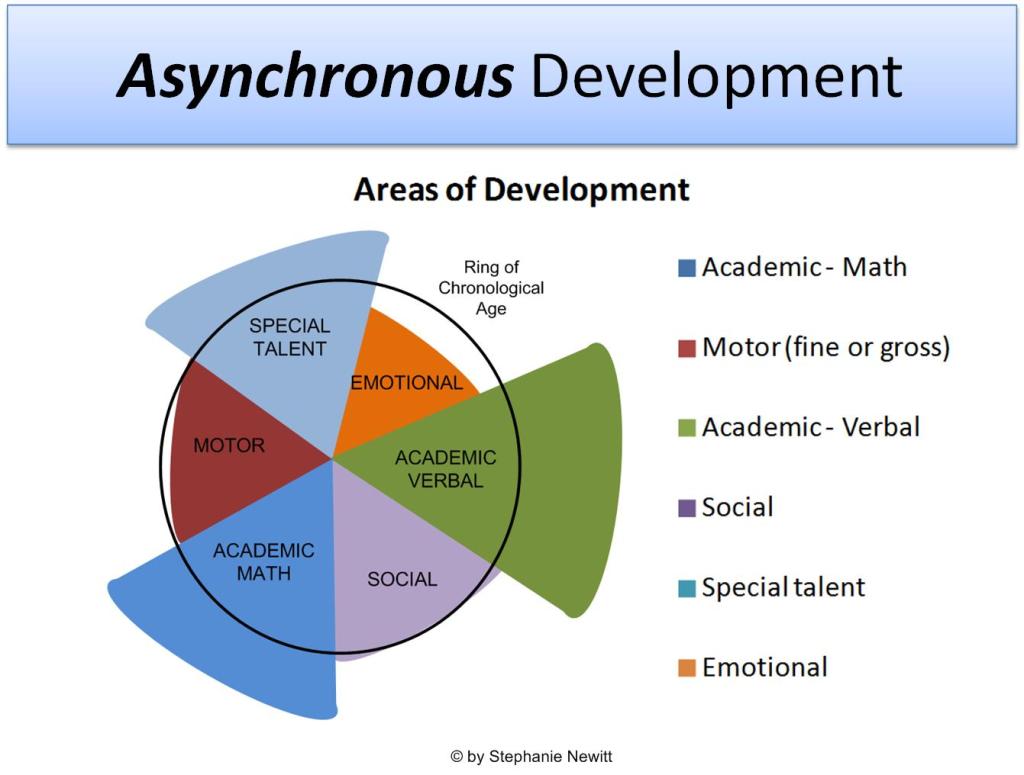
If a child is gifted in a narrow area, such as language, mathematics or science, there may some pressure by the parents to try to accelerate the learning in these areas. Promoting the child to an older class can potentially create some problems. Children develop different skills at different rates, and this is referred to as asynchronous development. For example, an 8-year-old child may have the language ability of a 14-year-old, and if they join a class of older children, their social and emotional development may be out of synchrony with the older children. One solution of this dilemma is to have special individual tuition devoted to the academic areas appropriate for that child.
A flexible individualised educational system is recommended. With technological advances in education, perhaps this pipe dream may be realised in the near future.
Multiple Intelligences
Another criticism of using conventional IQ tests for selecting students for the gifted education program is that it assesses a relatively narrow range of abilities, namely mathematics, language, and visuospatial. Howard Gardner originally suggested 7 intelligences in 1983, but he has increased this number to 9. They include:
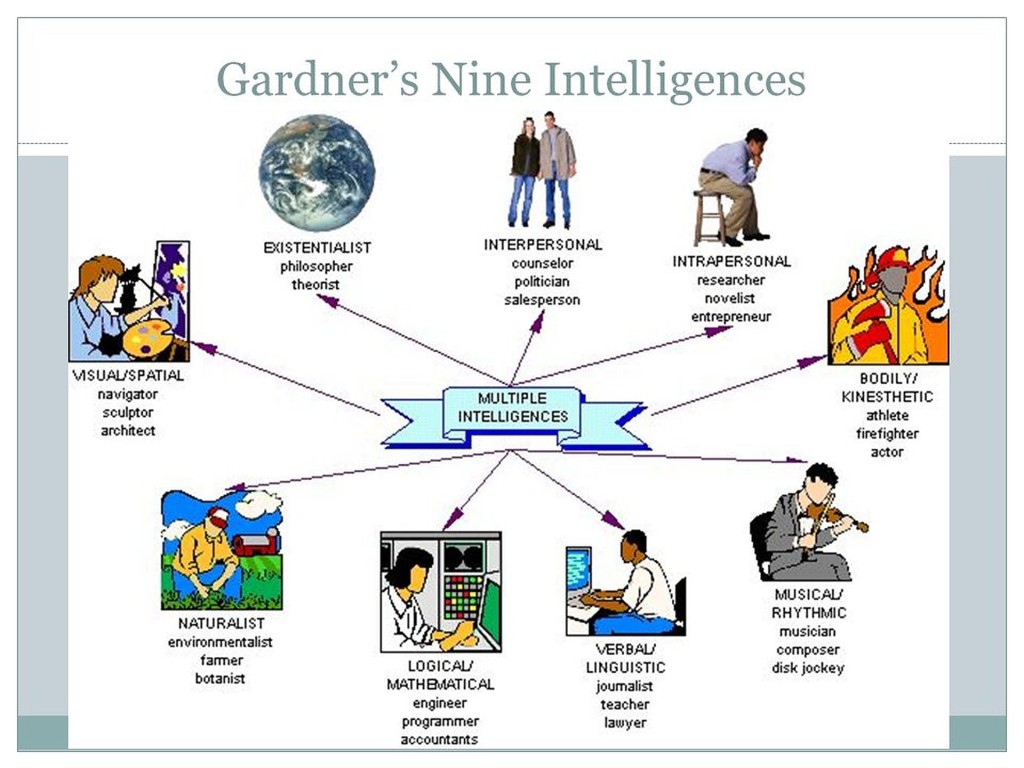
If we look at education more holistically, then gifted children who excel in only a few areas, should nevertheless be given the opportunity to explore other areas.
Problems of Gifted Children
Parents seek medical or psychological consultation for their gifted child because they might develop some challenges related or arising from their giftedness. These problems can arise not only in gifted students attending non-gifted classes, but also in those going to gifted classes. The problems include:
a) Attention Deficit Hyperactivity Disorder (ADHD)
The 6-year-old boy described in the opening paragraph, is one such example. The psychologist did a formal assessment, and found that he did not have ADHD, but instead he was gifted. The explanation of the restless behaviour, failure to pay attention, and his constantly interrupting the teacher, is attributed to his amazingly fast ability to learn. The teacher caters to the average student, and spends longer repeating the lesson, which bores the gifted student.
b) Disruptive Behaviour and Poor Social Skills
Some gifted children get so fed up with the slow pace of the teaching that they engage in other activities, like chatting with their neighbours. Others are perfectionists and keep on correcting their teachers or classmates when they say something deemed incorrect. Some gifted children have poor social skills and do not know how to interact with their peers. They may be perceived by their peers to be egoistical or arrogant, and this can lead to arguments, fights, and ostracization.
c) Depression
Depression and suicides are found in gifted children, but it is controversial whether or not it is more frequent in gifted children compared to their age-matched non-gifted peers. It has been suggested that gifted children are more prone to depression and suicide because they have heightened sensitivities, they tend to be introverted, overachieving perfectionists, or they become extremely worried if they do not fulfil their self-imposed high standards, and they may be prone to bullying by their non-gifted peers.
d) Twice-Exceptional
The term twice-exceptional refers to a person who is both gifted as well as being disabled. For example, it may be a person who has a very high IQ and is also autistic. The special needs may be a learning disability, dyslexia, attention deficit hyperactivity disorder, visual or hearing impairment, or motor deficits. If their accompanying disability is missed or ignored, these talented children may be under a lot of pressure, may lose motivation and therefore under-achieve.
Terman’s Termites

Lewis Terman (1877-1956) was the founder of the Stanford-Binet IQ test, which was introduced in 1916. In 1921 he began a longitudinal genetic study of highly gifted children, which were later dubbed as “Terman’s Termites”. They were followed up until they reached 70 to 80 years of age. Altogether he recruited 1,528 participants between the ages of 3 to 28, who had an IQ of >135, comprising 1% of the general population, which he defined as “genius”. There were 856 boys and 672 girls, mostly from California, and they were predominantly white and middle class. The finding was summarised as: “the gifted child becomes the gifted adult”. His Termites had ten times the national rate of earning a university bachelor’s degree of that era. A significant number of graduates went on to earn postgraduate degress: 57 doctors, 92 lawyers, and 97 PhD’s which was a high percentage of that time period. The salaries of his Termites was also significantly higher than the matched median per capita income.
It is of interest to note that two subjects rejected by Terman because their IQ fell below 135, went on to win a Nobel Prize each. Hence the joke suggesting that if you want to win a Nobel Prize, you should not have too high an IQ!
Lewis Terman recommended helping highly gifted children with special gifted education, trained teachers, employing enriched and accelerated curriculum. The benefits of this approach has been vindicated by more recent studies in several other countries.
Contemporary Gifted Persons

William James Sidis enrolled in Harvard University at the age of 9 years. He predicted the existence of regions of space where the second law of thermodynamics operated in reverse to the temporal direction.
Christopher Michael Hirata won the International Physics Olympiad at the age of 13 and graduated from Caltech at the age of 18. He is a leading exponent of precision cosmology, combining interdisciplinary computer studies, theoretical studies, and observational astronomy. His achievements are in the field of dark energy and the accelerating expansion of the universe.
Christopher Langan obtained a perfect SAT score but dropped out of university because he could teach his professors more than they could teach him. Langan has developed an idea he calls the “Cognitive-Theoretic Model of the Universe” which he maintains “explains the connection between mind and reality”.

Terence Tao is an Australian-American whose Hong Kong parents emigrated to Australia. He attended a university mathematics course at the age of 8 years, and co-authored over 300 research papers, including formulating the Green-Tao theorem for which he was awarded the Field Medal, which is considered the mathematics equivalent of the Nobel Prize. He is also referred to as the “Mozart of Maths”.
Kim Ung-Yong got his PhD degree at the age of 8 years. At the age of 15, he was doing research work for the National Aeronautics and Space Administration (NASA). He is currently the Vice President of North Kyeong-gi Development Research Center.
Philip Emeagwali is a Nigerian computer scientist whose simulation was the first program to apply a pseudo-time approach to reservoir modeling. At the age of 35 he received the Gordon Bell Prize for an application of the CM-2 massively-parallel computer.

Marilyn Vos Savant is an American magazine columnist, author, lecturer, and playwright.
Edith Stern graduated from university at the age of 15 and is an American inventor and mathematician. She holds over 100 USA patents, and was the former Vice-President for Research and Development at IBM.
Ainan Cawley is a Singaporean living in Malaysia. At the age of 8 years, he was attending a chemistry course at the Singapore Polytechnic, and at 9 years of age, he could memorize π (pi) to the first 518 decimal places. At the age of 12 he wrote the script and composed the music for a short film.
Conclusions
Gifted children are valuable human resources for any country. If nurtured appropriately and allowed to reach their maximum potential, they can contribute to the future of their country and the world.

References
Wikipedia. Intellectual giftedness.
https://en.wikipedia.org/wiki/Intellectual_giftedness
National Association for Gifted Children (USA). What is giftedness?
https://www.nagc.org/resources-publications/resources/what-giftedness
Davidson Institute. What is giftedness?
https://www.davidsongifted.org/gifted-blog/what-is-giftedness/
Wai J. What a century of research reveals about gifted kids.
https://www.psychologytoday.com/sg/blog/finding-the-next-einstein/201701/what-century-research-reveals-about-gifted-kids
Ministry of Education Singapore. Gifted education programme.
https://www.moe.gov.sg/programmes/gifted-education
Wikipedia. Gifted education programme (Singapore).
https://en.wikipedia.org/wiki/Gifted_Education_Programme_(Singapore)
Neihart M, Teo CT. Addressing the needs of the gifted in Singapore.
file:///D:/Medicine/Gifted/Gifted%20Education/Singapore%20Gifted%20Education%201.pdf
Neihart M, Tan LS. Gifted education in Singapore.
file:///D:/Medicine/Gifted/Gifted%20Education/Singapore%20Gifted%20Education%202.pdf
Eren F et al. Emotional and behavioral characteristics of gifted children and their families.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6060660/
Page JS. Challenges faced by “gifted learners” in school and beyond.
http://www.inquiriesjournal.com/articles/330/challenges-faced-by-gifted-learners-in-school-and-beyond
Gaille B. 15 Intelligence testing pros and cons
https://brandongaille.com/15-intelligence-testing-pros-and-cons/
Wikipedia. Theory of multiple intelligences.
https://en.wikipedia.org/wiki/Theory_of_multiple_intelligences
Transformations. Unexpected consequences of growing up gifted.
https://www.mytransformations.com/post/unexpected-consequences-of-growing-up-gifted
Warne RT. An evaluation (and vindication?) of Lewis Terman.
https://journals.sagepub.com/doi/pdf/10.1177/0016986218799433
Freeman J. Giftedness in the long term.
https://files.eric.ed.gov/fulltext/EJ746289.pdf
Written by Kenneth Lyen 19 July 2021

by Kenneth Lyen
Rise in Suicides
Today I learnt that one of my student’s close friend had committed suicide. And only a few months ago, one of my colleague’s son had also committed suicide. It is devastating for these families when their young ones, in their early 20s, end their lives.
The Straits Time of the 8 July reported that there were 452 suicides in Singapore in 2020 (1), and the Malay Mail of 29 June stated that in the first quarter of 2021 there were 631 suicides in Malaysia, far higher than in previous years (2). Why do people take their own lives? Is the increase in suicide rates related to the Covid-19 pandemic? I will discuss this later. But first I will examine depression.
What is Depression? (3,4)
It is a feeling of sadness that is felt more intensely and lasts longer than the transient heartaches, disappointments and blues that we all encounter in our daily lives.
Clinical Presentation
There’s a difference between “having depression” and “feeling sad”. We all feel very despondent when we fail an exam, get rejected by an institution of tertiary education, or lose our job. We feel sad, but after a while, we pull ourselves together and overcome this temporary unhappiness. In contrast, clinical depression lingers on for much longer, sometimes two weeks or more. It interferes significantly with our studying, working, playing, eating and sleeping.
Symptoms of depression
The following symptoms are listed in the American Psychiatric Association’s Diagnostic and Statistical Manual 5th Edition (DSM-V) (5):
Diagnosis
According to the DSM-V, you need five or more of the above symptoms to qualify for a diagnosis of depression, On top of that, there are the following additional requirements: these symptoms must cause significant distress to one’s daily life. They cannot be due to the consumption of medicines known to be associated with depression. One needs to exclude substance abuse, and other medical or mental conditions, such as a schizoaffective disorder. There cannot be a manic or hypomanic episode at any point.
Depression can affect men and women all the way from early childhood to old age. No socioeconomic status or ethnic groups are exempt from depression.
Other Symptoms Associated with Depression
We have listed above the official DSM-V symptoms of depression, but most people who have been working with individuals who suffer from this condition are aware of other symptoms listed below, and they should be looked out for:
How Depression Affects One’s Daily Life
There are many ways in which depression can affect one’s daily life. These include:
Depression in Children
Depression in children is quite difficult to pick up, and the diagnosis is often delayed or missed. Symptoms may not be constant, and can fluctuate from day to day, depending on the environment and events. As a child grows up, the manifestations of depression can unfold differently at different ages. One must have a high index of suspicion if a child has continuous feelings of sadness or hopelessness, if there are bouts of anger or crankiness, if they become socially withdrawn, display changes in appetite or food preferences, change their sleep patterns, have difficulty concentrating on schoolwork, cry a lot, or have thoughts of suicide. Some may even present with superficially unrelated symptoms like headaches and abdominal pain, so caregivers and doctors should be alert to the possibility of an underlying depression.
Subtypes of Depression
a) Peripartum Depression
Post-partum depression or “Baby Blues” usually occurs after childbirth, but studies have shown that some mothers may have depression prior to childbirth. Thus, the condition has been renamed “depressive disorder with peripartum onset”. It can occur during pregnancy or up to 4 weeks after birth. Some 10-15% of mothers experience postpartum depression. Symptoms include mood swings, frequent crying, trouble bonding with the baby, tiredness, a fear that they will not be a good mother, or a sense of worthlessness or shame. In women, several hormones including estrogen, progesterone, prolactin and cortisol all decrease significantly after childbirth, and this drop may be responsible for causing the depression. Lifestyle changes may also play a role, because men can also experience depression around the same time. In men, their levels of testosterone and vasopressin fluctuate during and immediately after their female partner’s pregnancy, but the precise mechanism of depression in males is still unclear. Both males and females will experience environmental changes such as dealing with an unconsolable baby, sleep deprivation, changes in one’s daily routines, and having difficulty finding adequate support to take care of baby.
b) Atypical Depression
Atypical depression is characterised by increased sensitivity and reactions to changes in the environment. There may be improved mood during positive events, and this is referred to as “mood reactivity”. This contrasts with “melancholic depression” where even previously pleasurable events do not elevate one’s moods. Atypical depression may exhibit increased appetite, weight gain, heavy feeling in the limbs (leaden paralysis), oversleeping, and and becoming extremely anxious when being scolded or rejected.
c) Persistent Depressive Disorder (Dysthymia)
This subtype is a chronic form of depression which lasts over longer periods of time usually more than 2 years. The severity can also fluctuate over time. Symptoms include changes in appetite, changes in sleep, fatigue or low energy, reduced self-esteem, reduced concentration, struggling to make decisions, feeling hopeless, and harbouring pessimistic thoughts.
Differential Diagnosis
Bipolar Disorder (6)
Bipolar disorder was formerly known as manic-depression, and is characterised by extreme mood swings between hyperexcitable behaviour followed by depression. Some patients are misdiagnosed as suffering from depression. One should try to find out if the person has up and down mood swings, and if there are manic episodes, then this points towards a diagnosis of bipolar disorder. The reason why it is important to make a correct diagnosis is that the treatment differs from depression. Lithium carbonate is the preferred treatment for bipolar disorder.
Seasonal Affective Disorder (SAD)
Depression that occurs either in the winter months or during spring-summer months are diagnosed as Seasonal Affective Disorder (SAD). In those countries where the winter months are cold and the sun sets early resulting in dark afternoons and evenings, can make some people feel rather moody and, as the acronym suggests, sad. It has recently been realised that there is also depression that can occur during the spring and summer months. It is thought that this form of depression is due to allergy to pollen.
Causes (7,8)
The causes of depression are still not fully worked out. There have been a lot of research being conducted utilising advanced technology, and the results are still coming in.
Genetics (9)
If a first degree relative has depression, then one has a higher risk of getting depression too. If an identical twin has depression, the other twin has a 60-80% chance of developing it. A non-identical twin, on the other hand only has a 20% chance of experiencing depression.
The vast majority of individuals suffering from depression do not have close relatives with this condition. Because depression is a heterogeneous condition often overlapping with other personality, behavioural and psychiatric disorders, and there are no laboratory or imaging techniques to make a definitive diagnosis, there is a problem. Is depression a single disease, or is it made up of several diseases with some common and some overlapping symptoms? Therefore, what exactly can one correlate any particular set of candidate genes with?
Unlike other major psychiatric disorders like autism, genetic studies have not achieved very promising results. Following the successful human genome project, where the entire human DNA was mapped out in 2003, several Genome Wide Associations Study (GWAS) have been conducted in many countries, using large sets of samples, including thousands of patients with different forms of depression, and meta-analyses of thousands of patients scrutinised. Unfortunately, all have failed to identify any specific gene loci responsible for the predisposition to depression.
Recently there have been some suggestions that perhaps mitochondrial dysfunction may play a role in the development of major depressive disorders. If true, this throws a spanner in the works!
Environmental Factors
Life Events
Tragic events, like the death of a family member, failing an exam, losing a job, getting divorced, can increase the chances of having depression. A traumatic childhood, sexual or psychological abuse, neglect, poverty, and unhealthy lifestyles, can also predispose one to develop depression later in life. The side effects of certain medicines, like corticosteroids, beta-blockers, and statins (treatment of high cholesterol levels), can result in depression. Recreational drugs, like amphetamines, can also lead to depression.
Based on a combination of genetic and environmental factors, it is postulated that depression has neurochemical and neurostructural aetiologies.
Neuropathology of Depression (10)
The commonest theory about the cause of depression is the theory of chemical imbalance in the brain, especially the lack of serotonin, the “feel good chemical”. This is based on the observation that raising the level of serotonin through medicines can alleviate symptoms of depression in some patients. However, this view does not really capture the complexity of depression.
a) Monoamine deficiency theory
The underlying basis of depression is low levels of serotonin, noradrenaline or dopamine, the monoamines. Each may have an impact on separate sets of symptoms:
If one of these monoamine neurotransmitters is down, it may lead to a specific set of symptoms felt by the patient.
Serotonin is thought to be a major player, and perhaps even regulating the other neurotransmitter systems.
Tryptophan depletion: this is the amino acid which the body uses to make proteins including serotonin. Its depletion can lead to symptoms of depression. It also links to DNA studies of depression.
b) Neural Growth and Connections Theory
In recent years, scientists have discovered that brain cell growth and connections may play a larger role in the cause of depression. The hippocampus tends to be much smaller in depressed patients. The hippocampus is the area of the brain that controls memories and emotions. The longer the person has been depressed, the smaller the hippocampus becomes. Stress may be the main trigger to decrease the number of new neurons in this area of the brain. When this area of the brain regenerates and new neurons are stimulated, the mood improves. Many drugs include those that affect serotonin levels, have an indirect effect on the growth of brain cells. Cells that secrete serotonin also secrete other chemicals that stimulate growth of new neurons or neurogenesis.
Investigations
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging shows structural changes in the brain, and this has shown that a part of the prefrontal cortex known as the ventromedial cortex is much smaller in depressed individuals. The ventromedial cortex enables an individual to be stimulated by positive rewards and experience pleasure. It also enables one to switch from one mood to another mood. The cells involved in this function are the glial cells which supplied nerve cells with energy, and the number of these cells is decreased.
Positron Emission Tomography (PET) Scan
Function Magnetic Resonance Imaging (fMRI)
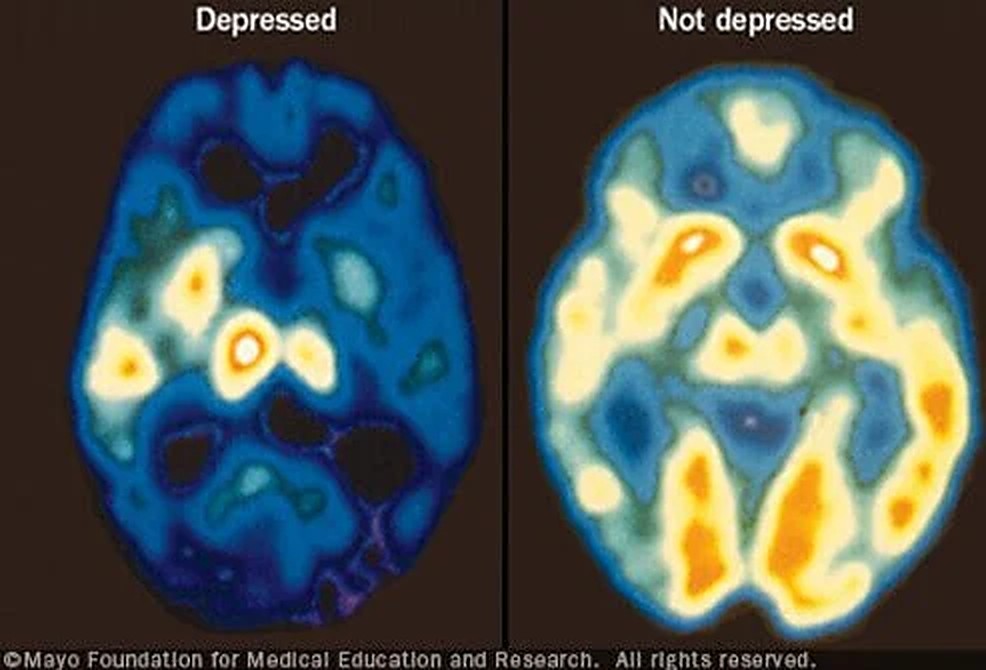
Positron Emission Tomography (PET) Scan allows scientists to determine the metabolic rates of the brain by measuring oxygen and blood sugar (glucose) utilization. Findings from PET scans have been confirmed by Functional MRI (fMRI). The latter looks at the blood flow into different areas of the brain. Using both these techniques, scientists have discovered that depressed people have less activity in the prefrontal cortex, including the ventromedial cortex. Paradoxically, there is more blood flow to the limbic area which contains the hippocampus, despite the shrinkage of the hippocampus in depression.
Electroencephalogram (EEG)
There can be changes in the rapid eye movement (REM) pattern as well as the slow wave phase of the sleep cycle. The EEG shows decreased REM sleep latency, decreased slow wave activity, and deeper delta waves in depressed subjects.
Blood Tests
Blood is taken to exclude hypothyroidism, high cortisol levels, vitamin deficiencies, and if consumption of recreational drugs (e.g. amphetamines) is suspected, blood can be taken to confirm their presence. Patients with high cholesterol levels might be taking statins, a potential cause of depression.
Treatments
Between 70-80% will improve their depressive symptoms if treated correctly. Whether or not antidepressants will lower suicide risk is a controversial topic; epidemiological studies have shown conflicting results, some showing increased and others showing decreased risk of suicide (28).
Antidepressants
a) Selective Serotonin Reuptake Inhibitors (SSRIs) (Citalopram, Escitalopram, Fluoxetine, Sertraline) (11)
This medicine blocks the reuptake of serotonin in the brain’s synaptic gap, and thereby prolongs the amount of serotonin in the synapse, enhancing neurotransmission. Serotonin is associated with happiness. SSRIs are generally preferred over other medicines, especially in children, adolescents, and late-onset depression. Adverse reactions are also less than other antidepressants. They include gastrointestinal upsets, sexual dysfunction, fatigue and restlessness. Citalopram when given in higher doses may cause prolongation of the cardiac QT interval.
In the 1990s, some 3% of American were taking Prozac, an SSRI antidepressant. The prevalence of consuming antidepressants has quadrupled over the following few decades, and there used to be a joke pointing to the United States as a “Prozac Nation”!
b) Serotonin/Noradrenaline Reupdate Inhibitors (SNRIs) (Veniafaxine, Desvenlafaxine, Duloxetine) (12)
For patients who suffer from pain or extreme tiredness, the SRNIs can be considered as a first-line treatment. SRNIs should be used alone because there are some interactions when combined with other antidepressants. Side effects include dizziness, dry mouth, diarrhoea or constipation.
c) Monoamine Oxidase Inhibitors (MAOIs) (Isocarboxacid, Phenelzine, Selegiline) (13)
Monoamine Oxidase Inhibitors prevent the metabolism of the monoamines 5-hydroxytryptamine (5HT) and noradrenaline, which increases the level of these neurotransmitter monoamines. An important side effect is that the risk of a hypertensive crisis. A low tyramine diet is recommended. Other side effects are insomnia, lack of sleep, anxiety, sexual dysfunction and weight gain.
d) Tricyclic Antidepressants (TCI) (Amitriptyline, Amoxapine, Desipramine) (14)
Tricyclic antidepressants block the reuptake of serotonin and noradrenaline in the presynaptic nerves. They were introduced in the 1950s and are currently used as a second line treatment when other antidepressants are ineffective. They elevate one’s mood. Unfortunately side effects are more common with TCIs, and include drowsiness, blurred vision, dry mouth, constipation, urine retention. They have also been used for people with obsessive-compulsive disorder and can help some who suffer panic disorders.
e) N-Methyl-D-aspartate (NMDA) Antagonists (Esketamine) (15)
The NMDA receptor is activated by glutamate and when that happens, a nerve signal is activated. The NMDA receptor antagonist will block the receptor and hence inhibits electrical impulses to pass. The antidepressant effects of the NMDA Receptor Antagonist can be felt relatively quickly, in about 4 hours.
ElectroConvulsive Therapy (ECT) (16)
A small and controlled amount of electric current is passed through the brain while the patient is under general anaesthesia. This induces a brief seizure. It has been around for decades and is used for major depressive patients. It is effective for about 50% of patients,
Deep Brain Stimulation (17)
Quite recently, neurosurgeons have reported successful treatment of several patients’ severe and treatment-resistant depression by implanting a wire with pacemaker-like device right into particular areas of the brain known as the subgenual cingulate region (also known as Brodmann’s area 25), and a part of the middle frontal cortex. The instrument delivers continual electrical stimulation to these brain areas, and this stimulation had a pronounced anti-depressant effect. Exactly why and how this treatment appears to work is unclear. Stimulation of these regions, which connects the limbic (emotion) centres in the brain with the frontal cortex can better manage and regulate one’s emotions. The frontal cortex might then help reduce depressive thoughts. Further research is in the pipeline.
Transcranial Magnetic Stimulation (18)
This is a noninvasive procedure using magnetic fields applied externally to stimulate part of the brain in order to alleviate depression. An electromagnetic coil delivers the magnetic waves to the frontal cortex. It is painless, safe and well-tolerated. The exact mechanism is unknown but it is speculated that the magnetic waves might stimulate that part of the brain which is underactive in people who have depression. Side effects are uncommon, and include headaches, twitching of the facial muscles, lightheadedness, and some tingling sensations. It works in about 30% of depressives, and fails in 50-60% of patients.
Non-Pharmacological Treatments
Psychotherapy (19)
Psychotherapy, or talk therapy, can help alleviate depression, and appears to be better in maintaining longterm alleviation. This includes cognitive behavioural therapy, interpersonal therapy, and psychodynamic therapy. They help the individual to focus on the present, and encourages the regaining of control over mood and function. Success for this type of therapy depends on the relationship between the patient and therapist.
Social Support
Love and support from family and friends helps tremendously. Strong social support leads to better longterm outcomes.
Music and Art Therapy (20,21)
Music and art therapy have both been shown to help people with depression. They make one feel more relaxed, they soothe the mind, and they lift one’s spirits.
Physical Activities (22)

Physical activities help reduce depression. Theories of why it works include the increased release of neurotransmitters, endorphins and endocannabinoids. Also tense muscles are relaxed. Exercising for 20 minutes x3 per week is effective.
Diet (23)
Although the evidence linking diet and relieving depression is not absolutely definitive, it is possible that eating more fruits and vegetables may have some benefits.
Suicide (24,25)

In Singapore, suicide is the leading cause of death for those aged 10-29. In 2020 there were 452 lives lost to suicide, amounting to 5 times more deaths from suicide than transport accidents (1). Males accounted for more than 70% of all suicides in 2020. For every suicide, at least 6 attempted suicide survivors are left behind.
The Risk Factors
Keep a lookout for risk factors. If you hear or observe any of the following, talk to the individual, asking how things are,
The Warning Signs
Listen Carefully
If you hear someone say anything like the following, take what they say seriously. Do not dismiss it summarily, and do not say “Everything will be all right”. Better to ask “Is there something bothering you?” “Are you unhappy about something?”
Unusual Actions or Writings
If you see someone doing the following or posting messages on the internet, it is better to err on the side of caution and discuss the matter with that person. “Anything the matter?” “Can we talk about what’s happening?”
Changes in Behaviour
The COVID-19 Pandemic and Depression (26,27)
From January 2020, the COVID-19 infection spread rapidly and engulfed the entire world. It changed all our lives. Millions of people have caught the disease, and already over 4 million people have died. Jobs are lost, affecting one’s income, schools and restaurants are restricted, theatre and music performances curtailed, reduced social mobility and social isolation, virtually no air travel, have all made people feel very lonely, and heightened stress, anxiety, frustrations, and hostility. It is estimated that a third of the population are anxious and depressed. Suicide rates have increased markedly (1,2).
At times like this, family, friends and social organisations need to support one another. Mental health counselling services need to be increased. Governments can help by ensuring COVID-19 is under public health control, encouraging vaccinations, and economically they can supplement lost incomes, reduce rental charges, opening up new jobs and training schemes.
Conclusions
It is important to note that suicide is preventable. Just talking to the depressed person can help alleviate suicidal thoughts and prevent a tragedy. Be neutral and do not be judgemental. Telling the person not to worry or that everything will sort itself out, is probably not going to help. Better to spend time listening to the person’s problems, worries, failures, suffering, and fears. Some individuals want to end their life because they want to terminate an unbearably painful situation, but if they can be shown an alternative solution, they may not embark on such an irreversible act. Sometimes you may have to talk to that person’s relatives or mutual friends to make them aware of the situation. If you feel you are not the right person to help, look for someone else who is more likely to be effective. Try to persuade the depressed person or their relatives to seek psychological or medical or any other appropriate help.
24-Hour Helpline: Samaritans of Singapore 1800 221 4444
Please do not lose hope!
References
1. Ng Keng Gene. Suicides reported in Singapore in 2020 amid Covid-19.
https://www.straitstimes.com/singapore/452-suicides-reported-in-singapore-in-2020-amid-covid-19-highest-since-2012
2. Jerry Choong. On average almost four suicide cases reported to police every day, Malaysia.
https://www.malaymail.com/news/malaysia/2021/06/29/covid-19-on-average-almost-four-suicide-cases-reported-to-police-every-day/1985906
3. Wikipedia. Major depressive disorder.
https://en.wikipedia.org/wiki/Major_depressive_disorder
4. eMedicine. Depression
https://emedicine.medscape.com/article/286759-overview#showall
5. Diagnostic and Statistical Manual 5th edition (DSM-V) Diagnosis of depression.
https://www.psycom.net/depression-definition-dsm-5-diagnostic-criteria/
6. Mayo Clinic. Bipolar disorder
https://www.mayoclinic.org/diseases-conditions/bipolar-disorder/symptoms-causes/syc-20355955
7. MentalHelp. Biology of depression.
https://www.mentalhelp.net/depression/biology-genetics-and-imaging/
8. Wikipedia. Biology of depression.
https://en.wikipedia.org/wiki/Biology_of_depression
9. Shadrina M et al. Genetic factors in major depression disorders.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065213/
10. Mayberg HS et al. Reciprocal Limbic-Cortical Function and Negative Mood: Converging PET Findings in Depression and Normal Sadnesshttps://ajp.psychiatryonline.org/doi/full/10.1176/ajp.156.5.675
11. UK NHS. Overview – Selective serotonin reuptake inhibitors (SSRIs)
https://www.nhs.uk/mental-health/talking-therapies-medicine-treatments/medicines-and-psychiatry/ssri-antidepressants/overview/
12. Medical News Today. What to know about serotonin-norepinephrine reuptake inhibitor (SNRI) drugs
https://www.medicalnewstoday.com/articles/snri#stopping
13. Ankrom S. How MAOIs work and common side effects.
https://www.verywellmind.com/monoamine-oxidase-inhibitors-maois-2584303
14. Ogbru A. Tricyclic antidepressants (TCAs).
https://www.rxlist.com/tricyclic_antidepressants_tcas/drug-class.htm
15. Pochwat B et al. An update on NMDA antagonists in depression
https://pubmed.ncbi.nlm.nih.gov/31328587/
16. American Psychiatric Association. What is ElectroConvulsive Therapy (ECT)?
https://www.psychiatry.org/patients-families/ect
17. ScienceDaily. Long-term study data shows Deep Brain Stimulation (DBS) is effective treatment for most severe form of depression.
https://www.sciencedaily.com/releases/2019/10/191004074901.htm
18. Mayo Clinic. Transcranial magnetic stimulation.
https://www.mayoclinic.org/tests-procedures/transcranial-magnetic-stimulation/about/pac-20384625
19. Cleveland Clinic. Psychotherapy for depression.
https://my.clevelandclinic.org/health/treatments/9300–psychotherapy-for-depression
20. MedicalNewsToday. What is music therapy and how does it work?
https://www.medicalnewstoday.com/articles/music-therapy#for-depression
21. VeryWellMind. What is art therapy?
https://www.verywellmind.com/what-is-art-therapy-2795755
22. Mayo Clinic. Depression and anxiety: exercise eases symptoms.
https://www.mayoclinic.org/diseases-conditions/depression/in-depth/depression-and-exercise/art-20046495
23. MedicalNewsToday. What foods are good for helping depression?
https://www.medicalnewstoday.com/articles/318428#vitamin-d
24. WebMD. Suicide.
https://www.medicinenet.com/suicide/article.htm
25. Suicide.org. How to help.
http://www.suicide.org/how-to-talk-to-suicidal-callers.html
26. US CDC. COVID-19 coping with stress.
https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
27. Duke-NUS. COVID-19: 1 in 3 adults anxious, depressed.
https://www.duke-nus.edu.sg/allnews/covid-19-1-in-3-adults-anxious-depressed
28. Wikipedia. Antidepressants and suicide risk.
https://en.wikipedia.org/wiki/Antidepressants_and_suicide_risk
Getting Help
National Care Hotline: 1800-202-6868 (8am to noon)
Mental Well-Being
Mental Health Helpline: 6389-2222 (24 hours)
Samaritans of Singapore: 1800-221-4444 (24 hours)
Singapore Association for Mental Health: 1800-283-7019 (Mon to Fri 9am to 6pm)
Silver Ribbon Singapore: 6386-1928, 6509-0271 (Mon to Fri 9am to 6pm)
Tinkle Friend: 1800-274-4788 (Mon to Fri 2:30 to 5pm)
Counselling
Touchline 1800-377-2252 (Mon to Fri 9am to 6pm)
Care Corner Counselling Centre (Mandarin): 1800-353-5800 (10am to 10pm)
Written by Kenneth Lyen 13 July 2021
by Kenneth Lyen
Introduction (1,2)
The commonest cause of dementia is Alzheimer Disease (AD), accounting for more than half the cases. It was first described by Alois Alzheimer when his patient, Auguste Deter saw him in a mental institution when she was 50 years old. She had lost her memory, screamed in the middle of the night, and was paranoid about her neighbours. She died at the age of 55, and autopsy of her brain showed senile plaques and neurofibrillary tangles.
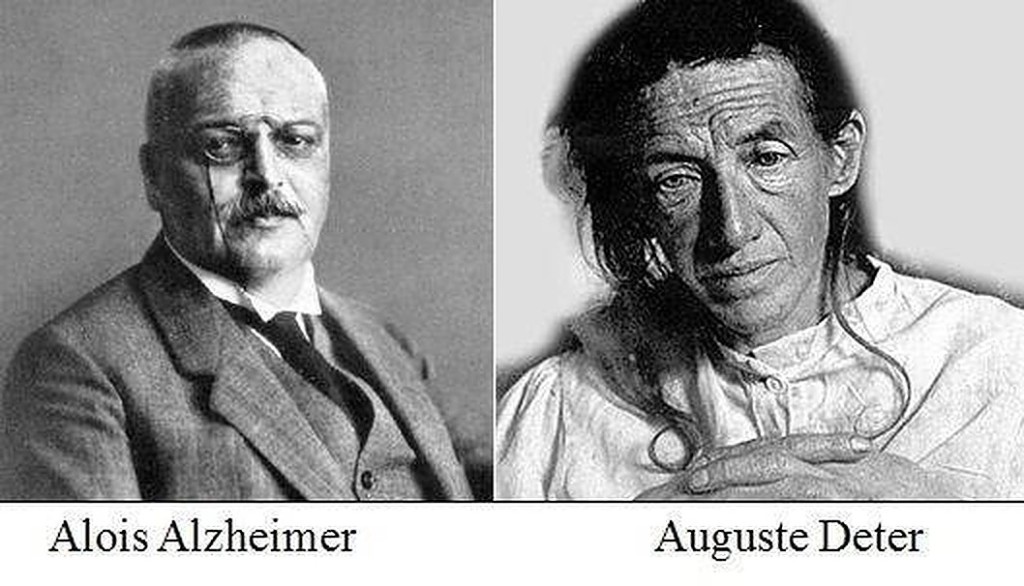
Symptoms
Alzheimer Disease does not come on suddenly or wipe out your memory in a short period of time. Instead, it is like a thief in the night that creeps up on you and over the course of years, slowly robs you of your powers of recall bit by bit. Quite often you are unaware that your mind is going downhill, until one day you meet an old friend and cannot remember their name.
Initially you might forget where you left your handphone, whether or not you switched off the air-conditioner, or what was the message you were supposed to deliver? Later you might forget what day it is, whereabouts you are, the names of your family members and even common everyday objects. Have you ever uttered the phrase: “It’s on the tip of my tongue”? You might keep on repeating the same questions over and over again. You might have mood swings, lose interest in things that used to captivate you, have difficulty sleeping, become irritated easily, get depressed, and withdraw from social interactions. (See Dementia article for more details).
Usually when symptoms become more severe, you or your relatives might decide to have you see a doctor.
Examination
The doctor will do a full and thorough physical examination. They will need to exclude diseases associated with dementia, such as hypothyroidism, hypertension, hypercholesterolaemia, diabetes, depression, alcoholism, Parkinson Disease, Huntington’s chorea, and cancer.
However, there are no specific abnormal physical signs in Alzheimer Disease. Of paramount importance the doctor has to do a careful cognitive assessment to test one’s memory (see Dementia article for more details).
Causes (3)
The pathological findings of Alzheimer Disease are amyloid plaques, neurofibrillary tangles, and cerebral atrophy. However, the causes of Alzheimer are still shrouded in mystery, but there are some interesting recent advances.
Amyloid Plaques
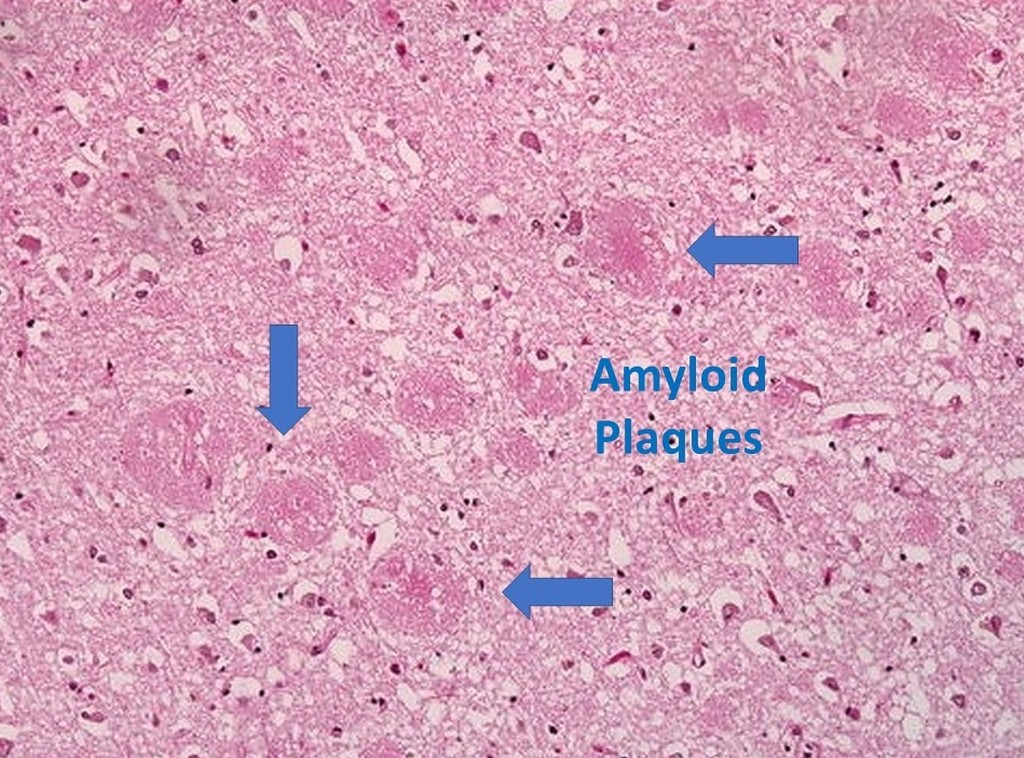
Amyloid plaques come from amyloid precursor protein (APP), a protein found in nerve membranes. Part of this protein sticks outwards through the nerve membrane, and the other part pokes inside the membrane. At a certain time, it is chopped off by a family of enzymes named secretases. Unfortunately one of the secretase members, called β-secretase, cuts the external part of the amyloid precursor protein in the wrong place, resulting in an insoluble fragment which will aggregate to form insoluble amyloid plaques.
Depending on where the plaques are located, they can cause different types of damage. If it is between synapses, it interferes with nerve transmission from one nerve cell to another. Amyloid plaques have the ability to activate microglia and astrocytes to release cytokines, hence inflaming the immune system to cause damage to the surrounding neurons. The plaques can also be found around blood vessels in the brain, where they can weaken the wall and predispose to haemorrhage.
Tau Proteins and Neurofibrillary Tangles
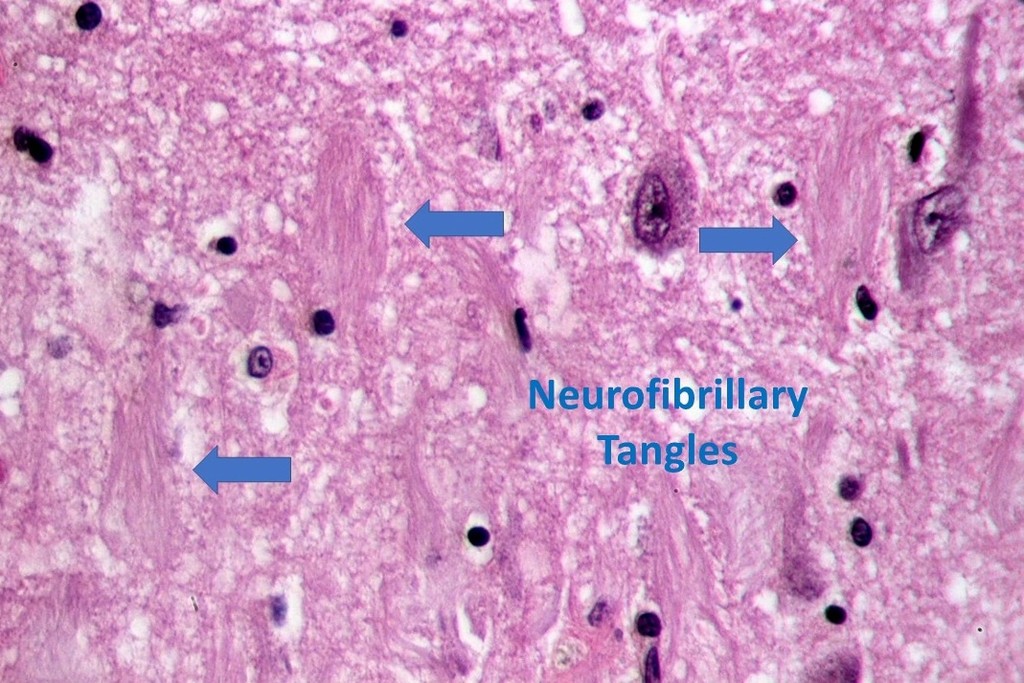
Inside nerve cells are microtubule cytoskeletons that hold up the neurons and prevent them from collapsing. These microtubules help shift nutrients and molecules along the neuron. Tau is a protein that holds the microtubules together and preserves their integrity. Somehow the external amyloid plaques send a signal into the neurons and activates kinase enzymes which phosphorylates the tau protein. These phosphorylated tau proteins leave the microtubules, and clump up with other tau proteins to form tangles, known as neurofibrillary tangles, which are located inside the nerve cells. As the neurotubules are no longer supported, they will collapse and the nervous impulses will not signal efficiently, and some of the nerve cells will die prematurely.
Genes (4-6)
When one person has Alzheimer Disease, a first degree relative such as a parent or a sibling, is more likely to be affected. There appears to be two major types of genetic risk factors: a) Monogenic, and b) Polygenic.
a) Monogenic
Monogenic Alzheimer Disease presents at a younger age-group, under 60 years old, and is less common, affecting less than 5% of all cases. Although they may be caused by hundreds of rare mutations, there are three major genes identified: the gene for the amyloid precursor protein (APP) located on chromosome 21, the presenilin 1 (PSEN1) gene located on chromosome 14, and the presenilin 2 (PSEN2) gene located on chromosome 1. How exactly they cause Alzheimer is still being investigated. Some of you may have noticed that chromosomes 21 and sometimes 14 are associated with Down Syndrome who can develop signs of dementia.
b) Polygenic
Polygenic Alzheimer cases present at an older age, greater than 60 years old, accounting for 95% of cases, most of which are sporadic. There is a complex polygenic factor, and there are nongenetic environmental factors. Although there is no one specific gene causing late-onset Alzheimer Disease, researchers have discovered a genetic variant of the apolipoprotein E (APOE) gene on chromosome 19. This discovery sparked a lot of interest because the APOE gene is also associated with the protein that carries cholesterol and other fats in the blood. Scientists are wondering whether there is a connection between Alzheimer Disease and vascular dementia, because they often co-exist in patients; and they ask what is the role played by the APOE gene?
Researchers have not found a specific gene that directly causes late-onset Alzheimer Disease. However, having a genetic variant of the APOE gene increases a person’s risk of developing Alzheimer’s. For example, a subtype of the APOE gene is the APOE e4 allele, and if you have two copies of this allele, it raises the risk of developing Alzheimer’s by up to 25%.
The human genome project was completed in 2003, and was a landmark in opening up the floodgates of genetic research. There is now a Global-Wide Association Study (GWAS) for Alzheimer Disease. Currently 600,000 individuals have been recruited, and a large number of gene variants have been discovered (7). When the results are analysed it will help in the early diagnosis of Alzheimer and can give us clues as to how to prevent or alter the progression of the disease.
Investigations
Blood Tests
Blood tests are taken to exclude suspected hypothyroidism, hypercholesterolaemia, liver and renal function, vitamin deficiencies, HIV-AIDS, and syphilis.
EEG (8,9)
Electroencephalography (EEG) shows abnormalities especially in severe Alzheimer Disease. When EEG is used on its own, it is not diagnostic of Alzheimer’s. When used in combination with other investigation methods, it enhances the diagnosis. EEG is helpful in distinguishing Lewy Body Dementia from Alzheimer Disease.
PET Scans
Positron Emission Tomographic scans are useful for the diagnosis of Alzheimer Disease not only when it is severe, but also in the early stages, known as Mild Cognitive Impairment (MCI). PET scans can also diagnose Lewy Body Dementia, Parkinson Disease and Fronto-Temporal Dementia.
There are two types of PET scans: a) Amyloid PET scans, and b) Tau PET scans.
a) Amyloid PET Scans (10)
Positron emission tomography scans use radioisotope compounds that bind to amyloid. They can be metabolised by the brain tissue surrounding the amyloid, which metabolise both the glucose and oxygen molecules which form part of these counpounds. And when that happens, it releases small amounts of positrons, which will then bump into some electrons. This encounter will generate two γ-rays which will fly off at 180° from each other. A series of γ-ray detectors placed correctly will detect the γ-rays.
Currently the most widely used radioisotope compounds are the fluoride radioisotope compound, 18Fluoro-Deoxy-Glucose (FDG), and 11C 2-(4′methylaminophenyl)-6-hydroxy-benzothiazole. The latter was made in Pittsburgh, and hence it was named Pittsburgh Compound B (PIB). Both are able to detect amyloid plaques in vivo and can therefore diagnose Alzheimer Disease (AD). But recent studies show that the PIB-PET scans are better able to distinguish the different degrees of severity in the milder forms of memory loss, known as Mild Cognitive Impairment (MCI) (see diagram below: naMCI = nonamnestic MCI, aMCI = amnestic or forgetful MCI).
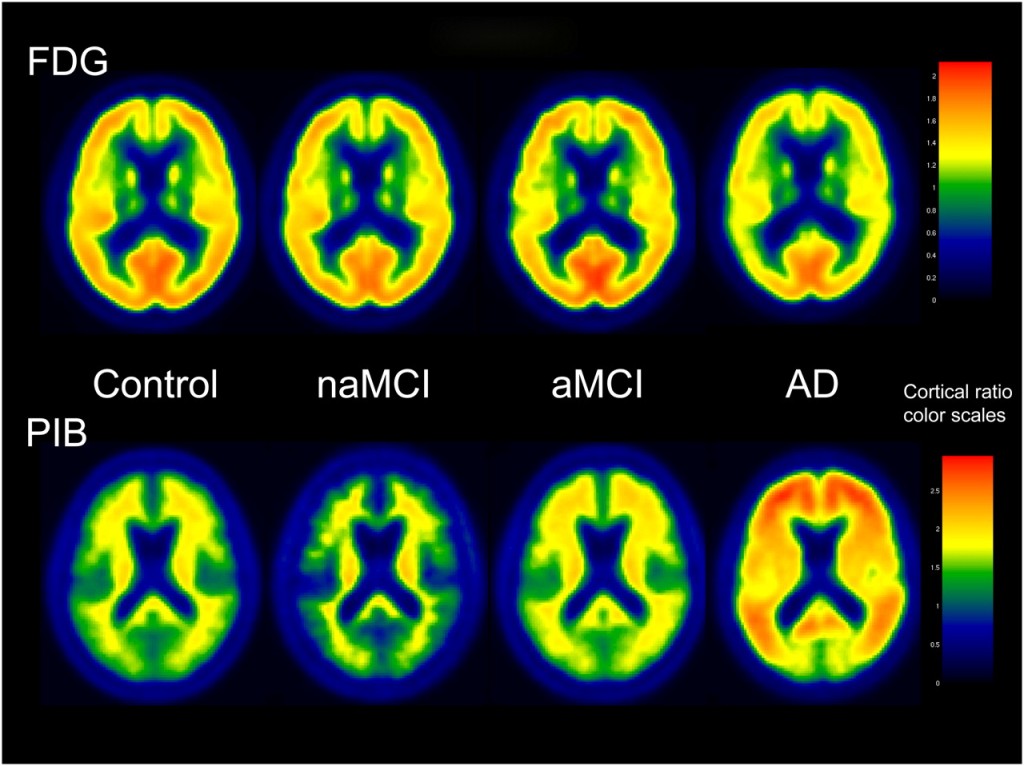
The PIB PET scans appear to be more useful for mild MCI dementia, as well as diagnosing the more severe Alzheimer Disease.
b) Tau PET Scans (11-13)
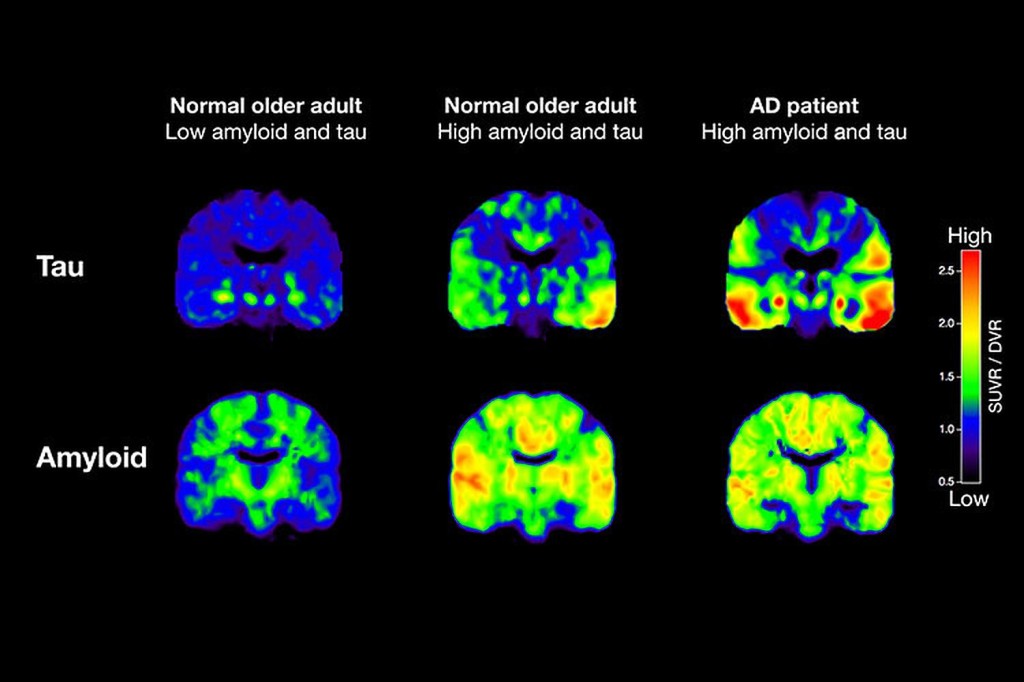
The tau PET scan uses the tracer lortaucipir/AV-1451 to detect the tau protein in the brain. In Alzheimer disease there is increased tau proteins. It appears that tau PET scans when used early, may be slightly better correlated with future brain atrophy compared to amyloid PET scans.
MRI Scans
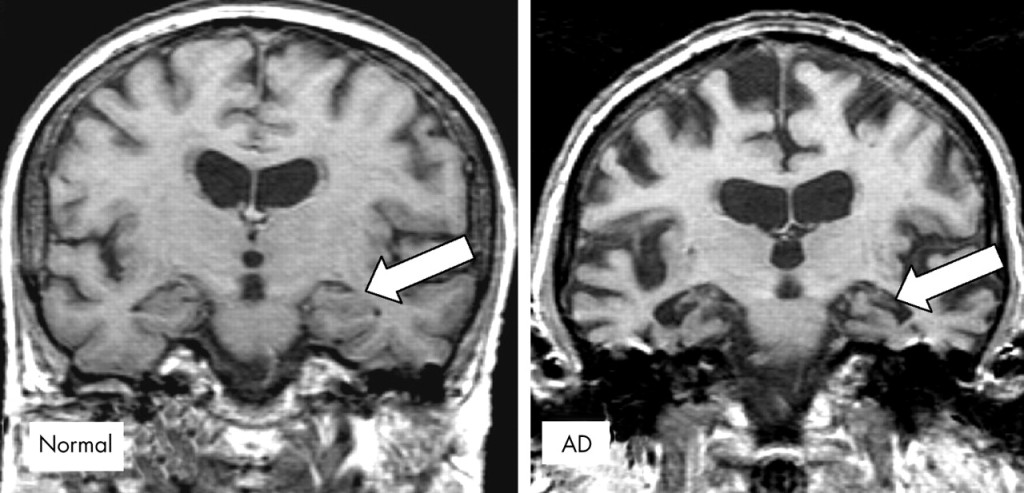
Magnetic Resonance Imaging (MRI) scans help diagnose Alzheimer by the shrinkage of the hippocampus (see arrow), coupled with signs of cerebral atrophy, such as deeper sulci and larger ventricles.
Cerebrospinal and other Fluid Biomarkers (14)
Amyloid and tau proteins can be detected in several biological fluids including the cerebrospinal fluid (CSF), and saliva. The most accurate correlation with Alzheimer Disease is the CSF amyloid and tau proteins. However, unlike PET scans, the fluid biomarker tests do not locate which parts of the brain are affected. Also doing a lumbar puncture to obtain CSF is uncomfortable or painful, and hence the procedure is not a popular choice.
Medical Treatment (15)
While there are no medicines that can cure Alzheimer Disease, there are a few drugs that can help in certain areas. They are described below:
Cholinesterase Inhibitors (Donepezil, Rivastigmine, Galantamine)
In Alzheimer Disease, the neurotransmitter acetylcholine is depleted. In normal circumstances, the level of acetylcholine is kept in check by the enzyme cholinesterase that breaks down any surpluses. But since the level of acetylcholine in Alzheimer patients is already low, studies were conducted to see if preserving what remains, by inhibiting cholinesterase, can make a difference. Yes, it probably helps. People taking cholinesterase inhibitors reported improved memory, think more clearly, and it helped them with daily activities. The exact mechanism of how the medicine works is still unknown. Side effects include loss of appetite, nausea, vomiting, diarrhoea, insomnia, nightmares, and heart arrhythmias.
N-Methyl-d-Aspartate (NMDA) Antagonists (Memantine)
Glutamate is one of the most abundant excitatory neurotransmitters in our body. One of the receptors that it activates is the NMDA receptor. While glutamate is an important neurotransmitter involved in many neurological functions including memory storage, too much is deleterious, and leads to nerve death. Memantine is a NMDA receptor antagonist, and helps regulate glutamate. It improves memory and learning. Side effects include dizziness, confusion, agitation, and headaches.
Antidepressants (Citalopram, Escitalopram, Venlafaxine) (16)
Many people with Alzheimer Disease also exhibit depression, which can exacerbate the ability to think, and can make daily living very challenging. They may become even more dependent on their care partner. Selective serotonin reuptake inhibitors (SSRIs) can be prescribed for depression as well as for Alzheimer Disease. SSRIs can alleviate depression, but side effects include weight gain, drowsiness, dizziness, blurred vision and nausea. Some studies have shown that long-term use of SSRIs might reduce dementia.
Anti-anxiety Drugs (Lorazepam, Diazepam)
Some Alzheimer patients also show anxiety under certain situations; they can get upset easily, and cannot keep still in any one place. Improving the environment by avoiding bright lights, loud noises, and clearing the room, can be helpful. If not, an anti-anxiety drug might sometimes reduce stress. However, some Alzheimer patients may become more confused, or become sleepy, have difficulty swallowing, and they may be at greater risk of falling down when moving about.
Antipsychotics (Olanzapine, Risperidone, Quetiapine)
If an Alzheimer patient is very aggressive, hostile, and suffer hallucinations, one might have to try one of the antipsychotic medicines. Preferably they should be used in limited situations for a short period of time. Side effects include heart problems, and some patients’ blood glucose can become elevated.
Controversial New Drug (17)
On 7 June 2021, the US Food and Drug Administration (FDA) approved a new drug, aducanumab (Aduhelm), designed to slow down cognitive decline in Alzheimer Disease. This is despite objections by the official FDA advisory committee. One of the late-stage clinical trials showed that there was no benefit. In contrast, two other trials, one on early-stage and another on late-stage Alzheimer Disease, showed that the drug helped. The FDA overruled their advisory committee and approved the drug, explaining that many Alzheimer patients were desperately wanting some form of treatment. Three members of the FDA advisory panel resigned over this issue.
Ineffective Treatments
A large number of herbal supplements, vitamins, dietary supplements have been proposed, but unfortunately none of them have been proven to work. This includes gingko biloba, vitamin E, B, and C, omega 3 fish oils, coenzyme Q10, curcumin, and polyphenols. Berries and nuts have also been advocated but they are also ineffective.
Other Therapies
Occupational and Physical Therapy
Occupational and physical therapists can help Alzheimer patients and their family in a variety of ways. These include training mobility and function, helping with communication and reasoning skills, and completing everyday tasks,. They can recommend labelling the different doors, getting hold of a dementia-friendly clock that can speak out the time and remind you what to do. They can introduce seating and mobility aids, and try out some of the newer technological aids (see below).
Speech Therapy
One of the major problems facing Alzheimer patients is their difficulty in communication, largely because of their memory loss. Speech therapy helps remind the individuals how to continue to use language. This includes repeating words, identifying pictures, and knowing what to say in different scenarios.
Music Therapy
It has often been shown that music helps Alzheimer patients by calming them down, making them feel happy. By singing songs, they are reminded of words for communication purposes. Music might also spur others into dancing, which becomes another form of exercise.
Daily Living Activities
Daily living activities might include, socialising, regular physical exercises, mental exercises, gardening, cooking, good nutrition, adequate sleep, learning a new language, and trying out new technologies,


New Technologies (18)
There are many new technologies that can help with a variety of functions, including:
The number of new devices and artificial intelligence devices are increasing rapidly.
Famous People with Alzheimer Disease
Below are some well-known public figures who developed Alzheimer Disease. Sadly, there are many more.
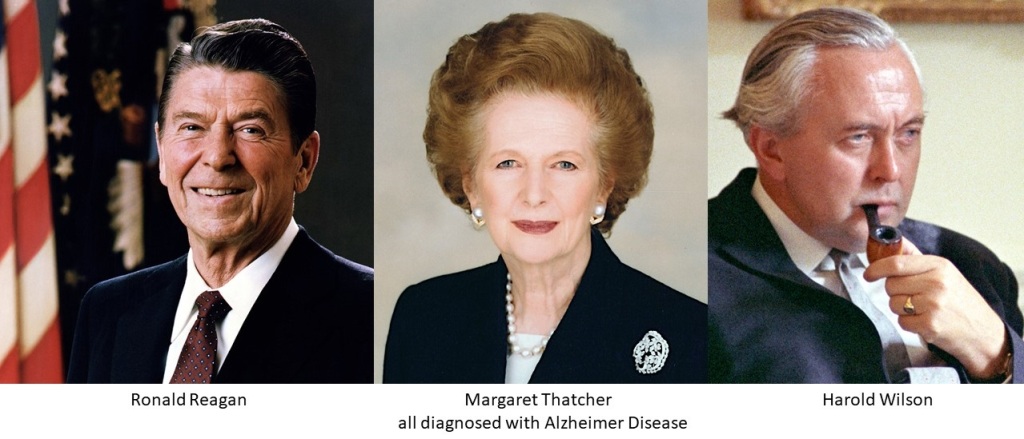
Can Alzheimer Disease be Reversed?
Scientists from Cambridge and Leeds have successfully fully reversed age-related memory loss in mice by reconstituting chondroitin 6-sulphate to their perineuronal nets. This paves the way for developing drugs that can prevent memory loss in humans when they age (19).
Conclusions
Alzheimer is the commonest cause of memory loss. There have been many advances in the diagnosis of the condition. To date the use of two classes of drugs, the anticholinesterase inhibitors, and the NMDA antagnoists have shown some promise in improving memory. The newest drug approved by the FDA has run into some controversy. It is hoped that in future we can better understand the pathophysiology of the condition and find new drugs that can prevent or even cure the disease.
Please see the Dementia and Memory articles that complement this review (20,21).
References
1 Wikipedia. Alzheimer’s Disease
https://en.wikipedia.org/wiki/Alzheimer%27s_disease
2 eMedicine. Alzheimer Disease
https://emedicine.medscape.com/article/1134817-overview#showall
3 Osmosis. Alzheimer Disease.
https://www.youtube.com/watch?v=nPT1nD6Wh6E&t=217s
4 Bagyinszky E et al. The genetics of Alzheimer’s disease.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3979693/
5 National Institutes of Health. Alzheimer’s Disease genetics fact sheet.
https://www.nia.nih.gov/health/alzheimers-disease-genetics-fact-sheet
6 Medline Plus. Alzheimer Disease (Genetics)
https://medlineplus.gov/genetics/condition/alzheimer-disease/#inheritance
7 Prokopenko D et al. Whole-genome sequencing reveals new Alzheimer’s disease–associated rare variants in loci related to synaptic function and neuronal development
https://doi.org/10.1002/alz.12319
8 Neiman ES. What EEG findings are characteristic of Alzheimer disease?
https://www.medscape.com/answers/1138235-192547/what-eeg-findings-are-characteristic-of-alzheimer-disease
9 Lee H et al. The EEG as a diagnostic tool in distinguishing between dementia with Lewy bodies and Alzheimer’s disease.
https://www.sciencedirect.com/science/article/abs/pii/S1388245714008384
10 Lowe VJ et al. Comparison of 18F-FDG and PiB PET in Cognitive Impairment
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2886669/
11 Weiler N. Alzheimer ‘tau’ protein far surpasses amyloid in predicting toll on brain tissue.
https://www.ucsf.edu/news/2019/12/416296/alzheimer-tau-protein-far-surpasses-amyloid-predicting-toll-brain-tissue
12 ALZ Forum. Tau PET Scans Turn Positive When Amyloid Does; Symptoms Follow
https://www.alzforum.org/news/conference-coverage/tau-pet-scans-turn-positive-when-amyloid-does-symptoms-follow
13 Alzheimer Drug Discovery Foundation. New PET scan detects tau tangles, additional changes in brains of Alzheimer’s patients.
https://www.alzdiscovery.org/news-room/announcements/new-pet-scan-detects-tau-tangles-additional-changes-in-brains-of-alzheimers-patients
14 Lee JC et al. Diagnosis of Alzheimer’s disease utilizing amyloid and tau as fluid biomarkers.
https://www.nature.com/articles/s12276-019-0250-2
15 Mayo Clinic. Understanding Alzheimer’s. Published by Meredith Corporation 2021.
16 Gramigna J. Long-term treatment with certain antidepressants may reduce dementia incidence.
https://www.healio.com/news/psychiatry/20200828/longterm-treatment-with-certain-antidepressants-may-reduce-dementia-incidence
17 McGinley L. FDA releases fresh details on internal debate over controversial Alzheimer’s drug.
https://www.washingtonpost.com/health/2021/06/22/aducanumab-aduhelm-alzheimers-drug-controversy-/
18 Allen K. Current Technology for Dementia and Alzheimer’s Disease.
https://www.brightfocus.org/alzheimers/article/current-technology-dementia-and-alzheimers-disease
19 Sujeong Yang et al. Chondroitin 6-sulphate is required for neuroplasticity and memory in ageing. Molecular Psychiatry https://www.nature.com/articles/s41380-021-01208-9
20 Lyen KR. Dementia. https://kenlyen.wordpress.com/2021/07/06/dementia/
21 Lyen KR. Memory. https://kenlyen.wordpress.com/2021/08/25/memory/
Written by Kenneth Lyen 6 July 2021. Revised 24 July 2021

by Kenneth Lyen
Introduction
Where did I leave my keys? Did I switch off the lights? What am I supposed to buy?
We all forget things, and as we get older, our memory deserts us. Memory loss is something that we are going to look forward to.
The brain is the most complex structure in the known universe. There are 86 billion neurons and 100 trillion connections between these neurons. For every second of our lives, thousands of nerve cells are firing off chemicals to control nearly every aspect of what we think or do. It is the damage of these nerve cells that can cause dementia.
The commonest cause of dementia is Alzheimer Disease. This will be discussed in greater detail in the article on Alzheimer.
Definition (1,2)
Dementia is the chronic acquired decline in memory and at least one other cognitive function…
… sufficient to affect one’s daily life.
Epidemiology
The prevalence of dementia increases with age.
| Age Range (years) | % Affected |
| 65-74 | 5% |
| 75-84 | 15-25% |
| >85 | 36-50% |
Although dementia affects mainly the elderly, it is actually not a normal part of ageing. According to the World Health Organisation, worldwide, there are around 50 million people who have dementia, and each year there are nearly 10 million new cases (3).
Causes of Dementia (4)
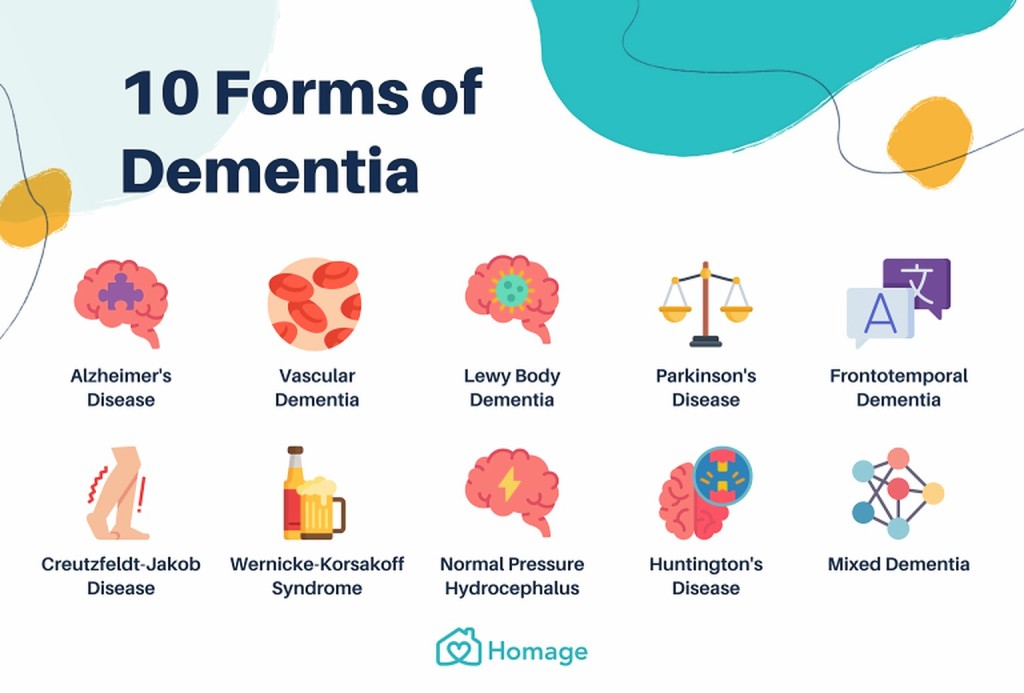
Dementia is an umbrella term that has several causes. Below are listed some of the causes:
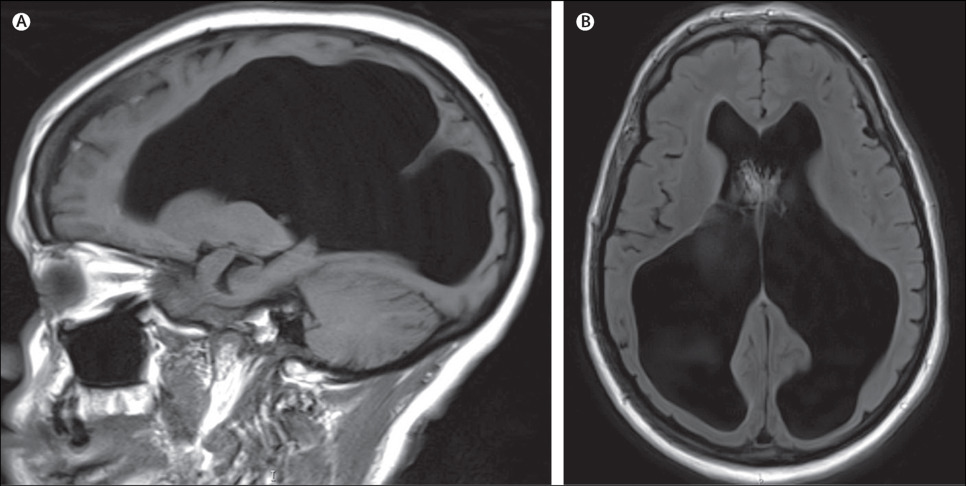

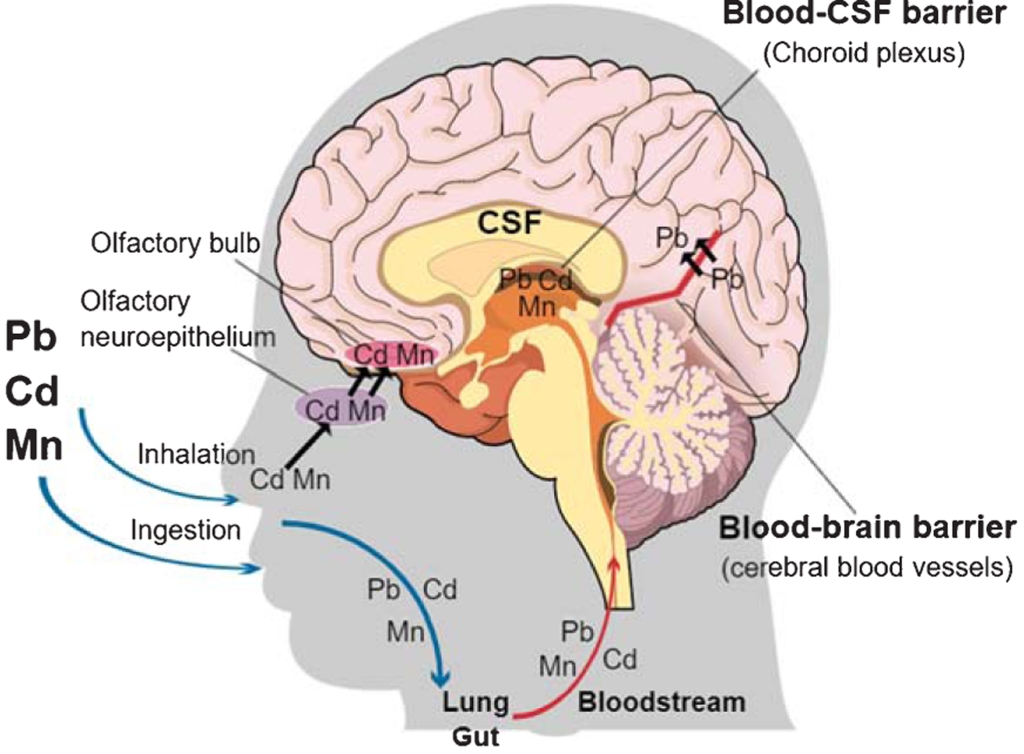




History Taking (5)
To verify the accuracy of the particulars, it would be good to have confirmatory information from a relative or the patient’s close friend. It might be necessary to interview the patient separately from the accompanying person.
While taking the history, one can simultaneously observe the behaviour of that person. Are they able to hear and see well, and are they behaving in the way expected for age? What were the initial symptoms? Was the memory loss like forgetting little things, forgetting appointments, or repeating the same questions? Were there any inappropriate behaviours? Did the symptoms worsen with time, and has it influenced their work and family life? Has it affected other activities like driving? One can assess their memory by asking their date of birth, their age, their address, and the name of the president or prime minister of a country.
One should ask about significant past illnesses, like high blood pressure, high cholesterol, diabetes, thyroid problems, etc. What medicines are they taking, and do they consume a lot of alcohol? Try to find out if the patient suffers from depression and anxiety. The family history should be explored, including whether other family members have Alzheimer disease, hypertension, cholesterol problems, thyroid conditions, cancer, and Huntington Chorea?
Examination
It is important to do a full general and neurological examination. Treatable causes of memory loss, like hypothyroidism, hypertension, Parkinson Disease and cancer should be excluded. The neurological examination includes how mentally alert the patient is, hearing and visual acuity, any tremors at rest, jerky movements. There may be clues during the examination that the individual is emotionally depressed or highly anxious.
A cognitive assessment should be carried out as follows:
These tests will help one decide if there is significant memory loss, and whether or not the patient needs to be referred to a psychologist for a more formal cognitive assessment.
Investigations (6)
Thyroid function, vitamin B12, folic acid, cholesterol levels, should be tested, and if human immunodeficiency virus (HIV-AIDS) or heavy metal poisoning is suspected, they should be tested as well.
An MRI Scan can show structural abnormalities and point towards Alzheimer disease, subdural haemorrhage, brain tumour, and other neurological conditions.
Proton Emission Tomography (PET) Scan can diagnose Alzheimer as well as Mild Cognitive Impairment (see Alzheimer article).
Onset of Dementia
Dementia does not come on quickly or suddenly. Instead, it is like a thief in the night that creeps up on you and over the course of years, and slowly robs you of your powers of recall bit by bit. Quite often you are unaware that your mind is going downhill, until one day you meet an old friend and cannot remember their name. It affects your work when you forget to carry out important tasks required in the workplace. You can upset your family members by failing to carry out your promises, especially if they have reminded you several times.
Mild Cognitive Impairment (MCI) (7)
Dementia is not an all or none phenomenon. It is a spectrum. When there is severe memory loss and behavioural problems, the diagnosis is clear. However, when symptoms are mild, and there may only be a few signs of dementia, but not enough to make a definitive diagnosis, then one is stuck in a limbo. This in-between state is known as Mild Cognitive Impairment (MCI) or Pre-Dementia.
MCI is further subdivided into the milder naMCI or nonamnesic MCI. These individuals are not amnesic and retain some memory. The other subdivision is the aMCI or amnesic MCI, and these people are forgetful, so they are considered slightly more severe on the dementia spectrum.

Management
The aims of management are several. Where possible one treats the underlying disorder or diagnosis. For example thyroxine is prescribed if hypothyroid is diagnosed. Similarly vitamin B12 is administered if deficient, and one should lower blood pressure, cholesterol levels, treat diabetes, Parkinson Disease, etc. If there is a subdural haematoma, intracranial bleeding, or a brain tumour, these need to be treated appropriately.
Medical treatment to reverse or cure Alzheimer Disease is not currently available. Several medicines have been produced, and some may have short-term improvements in memory. But none of them have proven to be effective over the long-term, as judged by large-scale scientific double-blind placebo-controlled trials. Recently the USA Food and Drug Administration has approved aducanumab (Aduhelm) for Alzheimer Disease, but there is some controversy (8). Other medicines for the treatment of conditions related to Alzheimer’s are described in the article on Alzheimer Disease.
Fortunately, there are nonmedical activities that have been shown to delay or perhaps slightly improve memory loss. These include:


Conclusions
Dementia is one of the major problems confronting the elderly, and the prevalence is increasing over the years. There are many causes of dementia, and if diagnosed and treated early, one might be able to mitigate some of the undesirable consequences. Currently the best ways of slowing down dementia is through nonmedical activities, including exercise, socialising, arts and crafts.
Please see the article on Alzheimer Disease and Memory that complements this review (10,11).
References
1. Wikipedia. Dementia. https://en.wikipedia.org/wiki/Dementia
2. eMedicineHealth. Dementia. https://www.emedicinehealth.com/dementia_overview/article_em.htm
3. WHO. Dementia
https://www.who.int/news-room/fact-sheets/detail/dementia
4. Mayo Clinic. Dementia.
https://www.mayoclinic.org/diseases-conditions/dementia/symptoms-causes/syc-20352013
5. Cooper S, Greene JDW. The clinical assessment of the patient with early dementia.
http://dx.doi.org/10.1136/jnnp.2005.081133
6. Bisaz R et al. The neurobiological bases of memory formation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4246028/
7. Hughes TF et al. Should mild cognitive impairment be subtyped?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3365571/
8. FDA releases fresh details on internal debate over controversial Alzheimer’s drug.
https://www.washingtonpost.com/health/2021/06/22/aducanumab-aduhelm-alzheimers-drug-controversy-/
9. Alzheimer Disease Association Singapore. https://alz.org.sg/dementia/singapore/a
10. Lyen KR. Alzheimer Disease. https://kenlyen.wordpress.com/2021/07/06/alzheimer-disease/
11. Lyen KR. Memory. https://kenlyen.wordpress.com/2021/08/25/memory/
Written by Kenneth Lyen 6 July 2021
by Kenneth Lyen
Attention Deficit Hyperactivity Disorder (ADHD) (1,2)
The maddening thing about ADHD is that most of us have some of the symptoms ascribed to this diagnosis. If you cannot sit still, you keep fidgeting with your fingers, your mind wanders, and you cannot pay attention and finish what you’re doing, then you might have ADHD. Hands up those of you who have these symptoms!
Diagnosis
The problem with making a diagnosis of ADHD is that it is a spectrum, and the boundary between normal and abnormal is very blur. There are no laboratory or brain imaging studies that are diagnostic, although some EEG changes may be helpful. Therefore, we rely almost exclusively on a constellation of symptoms and signs.
Children who present only with inattention without physical hyperactivity, are often missed, or their diagnosis delayed. It is only when school exam results come back below expectations, or teachers complain to the parents that their child is daydreaming, that the problem surfaces.
In contrast, children who are physically hyperactive and impulsive, might also be missed especially in boys, because it is natural for them to be energetic, aggressive and talkative. It is only the extreme end of the spectrum where the student loses their temper, injures someone else, or is at risk of being expelled from the preschool or school, that parents seek medical or psychological help.
Unfortunately, there is no single diagnostic test that can accurately and unequivocally diagnose ADHD. Doctors and psychologists can use one of the following rating scales to help them diagnose and track ADHD symptoms. A few examples are:
The DSM-V Test (3)
The American Psychiatric Association, in their Diagnostic and Statistical Manual 5th Edition (DSM-V) divides ADHD into two categories: a) Inattentive Type (used to be called Attention Deficit Disorder or ADD), and b) Hyperactivity and Impulsive Type.
a) Inattentive type
You need six (or five for people over 17 years) of the following symptoms that occur frequently, lasted for more than 6 months and found in at least two settings (eg school and home):
b) Hyperactive and Impulsive type
You need six (or five for people over 17 years) of the following symptoms that occur frequently, lasted for more than 6 months and found in at least two settings (eg school and home):

Differential Diagnosis
It is important to differentiate ADHD from conditions whose symptoms overlap. This includes thyrotoxicosis, where there can be inattention and hyperactivity. Another predisposition to inattention are some children who have dyslexia. When such children have difficulties reading and writing, they lose interest in their studies, and their mind wanders. It is important not to miss these diagnoses. There are comorbid conditions like autism spectrum disorder that one should be aware of.
Epidemiology (5)
Some 3% to 10% of the population have ADHD, making it one of the commonest neurodevelopmental disorders in the world. Because the diagnosis of ADHD is imprecise, the epidemiology can be quite variable. Take Singapore Institute of Mental Health study, for example (6). They quote a range of ADHD prevalence from 1.7% to 16%.
The ratio of males to females is just over 2:1 (7). The question is whether or not girls are underdiagnosed because they may be more equable less animated compared to boys?
Comparison of the epidemiology of ADHD in different countries are inconsistent. Some studies show now difference (8) between Asian compared to the Western countries. However, personal communications from many preschool and primary school teachers and principals observe that non-Asians tend to be more active in an Asian classroom.
Causes of ADHD
To explore the causes, one needs to define some of the components of ADHD. We need to ask many questions, including the following:
a) What is attention?
This is the ability to concentrate and maintain one’s attention. Looking at it from another point of view, it is the ability to filter out extraneous noise. Young children are more susceptible to inattention, and after a few years they can fix their attention quite well.
b) What is working memory?
Most people regard working memory synonymous with short term memory, but there is some debate about this. This is the ability to store an average of seven numbers, alphabets or words for 20-30 seconds. Recent studies have shown that working memory is stored in the prefrontal and parietal cortex.
c) What is executive function?
Executive function is a higher order ability for cognitive control, enabling one to reason, solve problems, organize, prioritize, and plan complex tasks. It involves the prefrontal cortex. The inability to take control of one’s activities and to prioritize, is one of the distinguishing features of loss of executive function. There is considerable overlap between this and ADHD. Most people with ADHD will have impaired executive function, although some people with loss of executive function do not have ADHD. However, understanding the relationship between the two can help in exploring the pathophysiology of ADHD.
Genetics (9,10)
Twin studies indicate that the hereditability of the disorder is between 60% to 80%. If a child has ADHD, the likelihood of one of the parents having the condition is 50%. And if the child is diagnosed with ADHD, the chances of a sibling also having the same diagnosis is 30%, which compares with a 3% to 10% risk in the general population.
To date there are no predominant gene mutations thought to cause ADHD. Large numbers of gene variations have been discovered to be associated with ADHD. Some are quite interesting, especially those that are involved in dopamine neurotransmission. Another interesting finding is that there seems to be an equal distribution of the gene mutations between males and females.
Brain Imaging (11)
Magnetic resonance imaging (MRI) and the more recent functional magnetic resonance imaging (fMRI) scans of the brain have helped delineate the anatomical and functional areas of the brain affected by ADHD. The following areas have been implicated:
a) Frontal cortex: this is involved in high level functions, including attention, and executive function.
b) Limbic System: this regulates emotions and attention.
c) Basal ganglia: deficiency of this area can cause inter-brain communication and information to short-circuit, and contribute towards ADHD.
d) Reticular activating system: this major relay system allows many pathways to enter and leave the brain; deficiency can cause inattention and hyperactivity.
Electroencephalogrphy (EEG) (12)
The EEG of ADHD shows an increase in theta slow wave in the fronto-central electrodes. It helps reinforce the clinical diagnosis of ADHD, but by themselves, the EEG is not sufficient to establish a definitive diagnosis.
Neurotransmitters (13)
Low levels of two neurotransmitters, noradrenaline and dopamine, have been found in some areas of the brain. Lack of these neurotransmitters can decrease conduction of neurones, and understanding the mechanism can help explain the drug treatment of ADHD.
Environmental Causes and Diets
Known factors predisposing to hyperactive behavior include genetic influences, or children who’s mothers drank alcohol heavily during their pregnancy, or were taking illicit or addictive drugs, or were heavy smokers.
Brain injury either from trauma, strokes, or meningoencephalitis (infections of the brain) are also associated with ADHD.
Intolerance or allergy to certain foods or drinks, such as milk, shellfish, sugar and wheat, are thought to produce hyperactivity in some children. There is anecdotal evidence that food additives, such as artificial coloring, preservatives and flavors, may contribute toward hyperactive behavior. However there is no good evidence that food or food additives can cause ADHD. Toxic pollutants such as lead, mercury, cadmium, insecticides, and herbicides, have also been postulated as potential causes, but they remain unproven. While we do not recommend any special diet to treat ADHD, and as long as the diet is safe, we do not stop parents trying out diets like avoiding sugars, or going on a gluten-free diet.
Comorbidities (14)
Because ADHD is so common, it would be expected that it might coexist with other conditions. There are quite a number of these comorbid conditions associated with ADHD, and they are listed here: anxiety, depression, autism, bipolar disorder, dyslexia, oppositional defiant disorder, obsessive compulsive and tic disorders. They often make the diagnosis of ADHD harder, especially if the comorbid symptoms are more apparent.
Treatment (15)
For mild ADHD, and for parents who refuse medications, the management of ADHD is behavioural therapy.
For more severe cases, there are several medicines available. The commonest medicine used is methylphenidate.
Methylphenidate is a stimulant drug that blocks the reuptake of dopamine and noradrenaline by neurons. The short-acting (Ritalin) is given orally and effects are noticeable within half an hour, and the effects last from 4 to 6 hours. The long-acting slow-release (Concerta) starts acting after 1 hour and it lasts from 8 to 12 hours. Side effects include loss of appetite, loss of sleep, anxiety, nervousness and nausea. When given with or after food, appetite is not affected. When administered in the daytime and avoiding giving it at night, there is no loss of sleep.
If teachers are not informed the student is taking methylphenidate and the parents quiz them to find if there are any changes in behaviour, most will answer positively. The students are often better behaved, less hyperactive, study longer, and exam results show significant improvements.
If a child is unable to take methylphenidate, the alternative is atomoxetine (Strattera). This is a noradrenaline reuptake inhibitor by neurons. It is better tolerated than methylphenidate, but it is less effective. Most of the side effects are gastrointestinal, including nausea, vomiting, heartburn, loss of appetite, and weight loss.
As a child gets older, the ADHD becomes less prominent, and some are able to stop medication. However, ADHD is a lifelong condition, and many continue taking medicines for quite a long time.
Strategies for the Home Management
Children with hyperactivity can learn to keep in check certain facets of their behavior. Parents need to draw up and implement a system of rules and rewards. They should also try to recognise their child’s strengths and weaknesses in order to help them build up their own self-regard and assurance. Try the following strategies:
Establish a few consistent rules of conduct. Phrase these rules positively in terms of what your child is expected to do. If these rules are broken, deal with them immediately with a set of actions that you have previously worked out. You should have a set of “deterrents” that you and your spouse have agreed upon, and you must not display disagreements on their imposition in front of your child.
Praise your child and reward them for good behavior. Hyperactive children tend to respond well to a structured system of rewards for good behavior. By awarding points for preferred behavior and subtracting points for undesirable conduct, this system encourages the child to earn privileges or rewards through better behavior. You can make charts or use stickers to demonstrate the results of good behavior. Try to concentrate on a few behaviors at a time. Additional behaviors can be tackled as others are controlled.
For the older child, draw up a written contract with your child whereby he promises to do their homework every day or exhibits certain desired behaviors. On completion of the task or adherence to the behavior, the child can choose certain privileges, such as the right to watch a particular television program. If your child fails to discharge their side of the contract, the promised privilege can be withdrawn.
Provide a time-out place for your child to go to when he or she is unmanageable. This should not be seen as a location for punishment, but rather as a place the child uses to cool off. The best place is probably the child’s bedroom. Just ensure that the place is safe for the child. Younger children may have to be instructed to go to the time-out location, but older children should realize themselves when they need to cool off and go on their own.
Create an area free from distractions and specify a time every day for your child to do homework. He should not be permitted to watch TV or listen to loud rock music while doing homework.
Keep a calendar of long-term plans and stick it on the refrigerator door or noticeboard.
Make your child write in a notebook what homework the teacher has set, and check it every night to ensure that it has been done.
In general, adopt positive strategies such as using praise and rewards. Do not expose or dwell upon your child’s weaknesses. Instead, you should help your child build their personal strengths. Avoid using sarcasm, mockery, or hostility. It only makes them feel dejected when told: “it’s so easy, anyone can do it.” Short, mild rebukes can help them focus their mind.
Prognosis
It used to be thought that children will totally grow out of their hyperactive behavior. Some symptoms, such as attention deficit, will improve with age. However, there is evidence that just over half the children with hyperactivity will continue to experience related problems as adults.
Many adolescents with hyperactivity lag behind their peers academically and are more prone to substance abuse and antisocial ats. Hence, psychological services and support should be provided throughout the entire period of the hyperactive child’s schooling. Smaller class sizes enabling teachers to give more individualized attention, discovering and encouraging special skills in art, music and sports, can also help the hyperactive child.
Any Advantages to Having Attention Deficit Hyperactivity?
According to Hallowell and Ratey, individuals with ADHD tend to be warm, creative, flexible, loyal, innovative and hard-working. Unfortunately, if their hyperactivity is too severe, they may not have the opportunity to express these positive qualities. An interesting observation is that many hyperactive individuals are creative and excel in the arts, entrepreneurship, entertainment, inventions, etc. Below is a picture of some famous people who are believed to have ADHD.
History of ADHD
Hyperactive behavior is a condition which can be traced back to ancient times. Research into this condition was first documented in the early 1900s by the English physician, George Still. He thought that hyperactive behavior was due to brain problems rather than moral failing, which was the prevailing attitude of that era. During the 20th century, many labels and definitions of the disorder have come and gone. These include “minimal brain damage, minimal brain dysfunction, hyperkinetic reaction of childhood, defect in moral control, post-encephalitic disorder, and hyperkinesis.” Current diagnostic changes have revolved around delineating the disorder according to whether the symptom of inattention exists with or without the symptom of hyperactivity.
Famous People with ADHD (16,17)
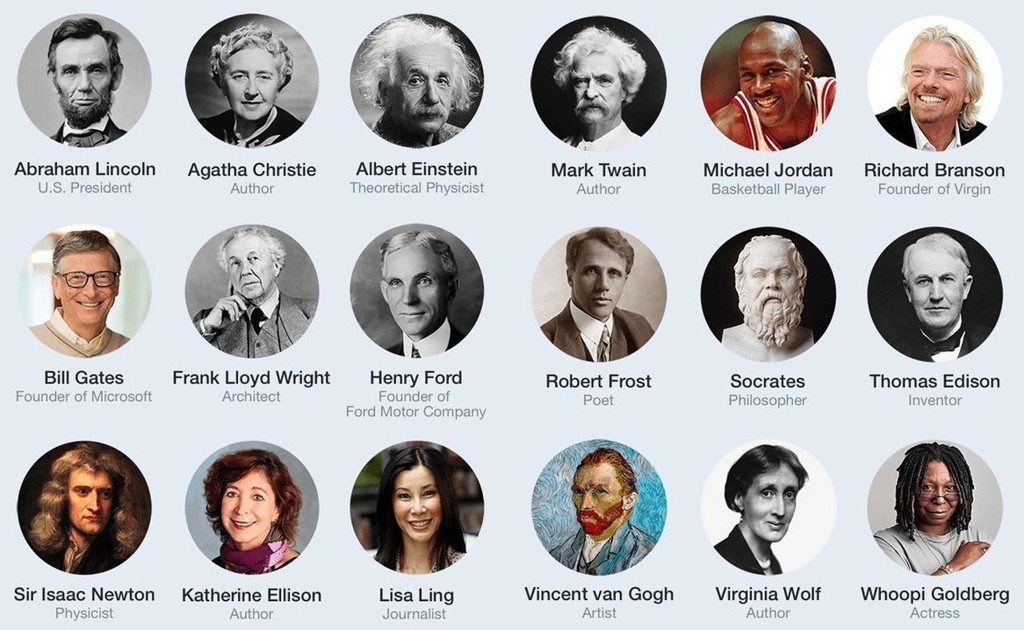
It is impossible to prove whether whose people who are no longer with us, really had ADHD. Richard Branson, the founder of the Virgin Group, is a self-confessed ADHD, although it has not been officially diagnosed. It is postulated that when your mind is overactive, you tend to think of a wider range of topics. If you link disparate ideas together, you might stumble upon something truly original. Creativity is the hallmark of the above famous people, and we would not be surprised that they have exploited ADHD as a gift that leads them to become a genius.
A question you might ask, is whether or not treating these people’s ADHD might rob them of their achievements?
Conclusions
ADHD is one of the most fascinating conditions that nearly all of us will encounter in our lives. It can affect our friends, colleagues, families, and sometimes even ourselves! There are so many unknowns and unexplored paths. The diagnosis is nebulous, the causes are largely undetermined, how medicines exert their actions are controversial, and why do so many people with ADHD go on to achieve so much in their lives? The author proposes that one could borrow techniques used in computerized gait analysis and combine it with continuous video recording, to derive an index of motor hyperactivity. These data can then be added to results of psychological testing. A composite picture can then be derived which will not only assist in the diagnosis, but will also help in measuring the degree of hyperactivity. There is obviously a lot more work to do before we can understand more fully the cause and management of this challenging condition. For the curious-minded, ADHD is an ocean worth exploring for the hidden treasures scattered all over.
References
1 Medscape. ADHD
https://emedicine.medscape.com/article/289350-overview#showall
2 Wikipedia: ADHD
https://en.wikipedia.org/wiki/Attention_deficit_hyperactivity_disorder
3 CDC. American Psychiatric Association Diagnostic and Statistical Manual 5th edition (DSM-V) test for ADHD
https://www.cdc.gov/ncbddd/adhd/diagnosis.html
4 The Test of Variables of Attention (TOVA)
https://www.tovatest.com/
5 CHADD. General prevalence of ADHD.
https://chadd.org/about-adhd/general-prevalence/
6 Singapore Institute of Mental Health. Brain-computer interface study.
https://www.imh.com.sg/research/page.aspx?id=894
7 Ramdekkar UP et al. Sex and age differences in attention-deficit/hyperactivity disorder symptoms and diagnoses.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3101894/
8 Liu A et al. The prevalence of attention deficit/hyperactivity disorder among Chinese children and adolescents
https://www.nature.com/articles/s41598-018-29488-2
9 Nichols H. Is ADHD genetic?
https://www.medicalnewstoday.com/articles/325594#is-adhd-genetic
10 Thapar A. Discoveries on the genetics of ADHD in the 21st century
https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2018.18040383
11 Paloyelis Y et al. Functional magnetic resonance imaging in attention deficit hyperactivity disorder (ADHD).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3763932/
12 Lenartowitz K, Loo SK. Use of EEG to diagnose ADHD.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4633088/
13 Silver L. ADHD Neuroscience 101.
https://www.additudemag.com/adhd-neuroscience-101/
14 ADDitude. When It’s Not Just ADHD: Symptoms of Comorbid Conditions
https://www.additudemag.com/when-its-not-just-adhd/
15 British National Health Service (NHS). Treatment attention deficit hyperactivity disorder.
https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/treatment/
16 Goodman DW. Famous people with ADHD.
https://addadult.com/add-education-center/famous-people-with-adhd/
17 Montijo S. 33 famous faces of ADHD
https://greatist.com/health/adhd-celebrities#historical-figures-with-adhd
Written by Kenneth Lyen
24 June 2021

by Kenneth Lyen
Definition of Dyslexia
The International Dyslexia Association defines dyslexia as a condition marked by difficulties with accurate and/or fluent word recognition and by poor spelling and decoding abilities (1). It is the commonest neurodevelopmental disorder.
Dyslexia is a lifelong condition characterised by difficulties in reading, spelling and writing. It is a problem of understanding and working with language. Because reading and writing forms a major component of our educational system, children who are slow in learning to read are often labelled as having a learning disability. Dyslexics often jumble up their letters and have difficulty associating a sound with a letter, such that even familiar words are difficult to read. There is quite a wide spectrum of dyslexia, ranging from mild to severe difficulties in reading, listening to words, spelling and writing. Dyslexia is not linked to intelligence, but difficulty reading instructions can affect the intelligence testing.
Developmental Language Disorder (DLD) (Diagnostic and Statistical Manual 5th Edition DSM-V) (2)
There is another condition with symptoms that overlap with dyslexia, but is now considered a separate entity. Known as Developmental Language Disorder (DLD), these children have no, or hardly any problems recognising words, but they cannot understand their meaning. DLD was previously known as Specific Language Impairment (SLI). Originally it was thought that DLD was part of dyslexia, but a less severe form, appearing in slightly older children.
The difference between these two conditions, is that the main problem of dyslexics is their inability to decipher the sounds of words and connect them with the visual written words. DLD, in contrast, can hear and see the words but cannot interpret what they mean. Thus they are thought to have problems with semantics (the meaning of words), syntax (the arrangements of words and phrases), and discourse (the formal orderly expression of thoughts delivered through speech or writing). DLD is therefore considered to be a higher level of processing deficit.
Dyslexia vs Developmental Language Disorder (DLD)?
In the past, it was thought that dyslexia and DLD were part and parcel of the same language disorder. Both conditions shared a core problem underlying the learning to read, which is phonology, or the ability to accurate hear phonemes (perceptually distinct units of speech sounds). Indeed both dyslexia and DLD do share difficulties with hearing these speech sounds. However, dyslexia was thought to be more severely affected in this area, and it was confirmed by testing using non-word sounds that the subject had to repeat. Dyslexics had greater difficulty repeating these sounds, and because they were unable to distinguish these phonemes, they would therefore have difficulty connecting sounds to the written language. And hence they would have difficulties reading and writing as a result.
In contrast, DLD individuals usually have less problems with phonology, and their predominant disability is in the comprehension of spoken or written language. To put it another way, their difficulty is in coping with broader oral language skills, including vocabulary and grammar, which are components of reading comprehension. Because learning to read tends to be later than learning to talk, DLD tends to be diagnosed later, when the children attend nursery class or kindergarten.
The distinction between dyslexia and DLD is depicted by the two-dimension model of Bishop and Snowling (3):
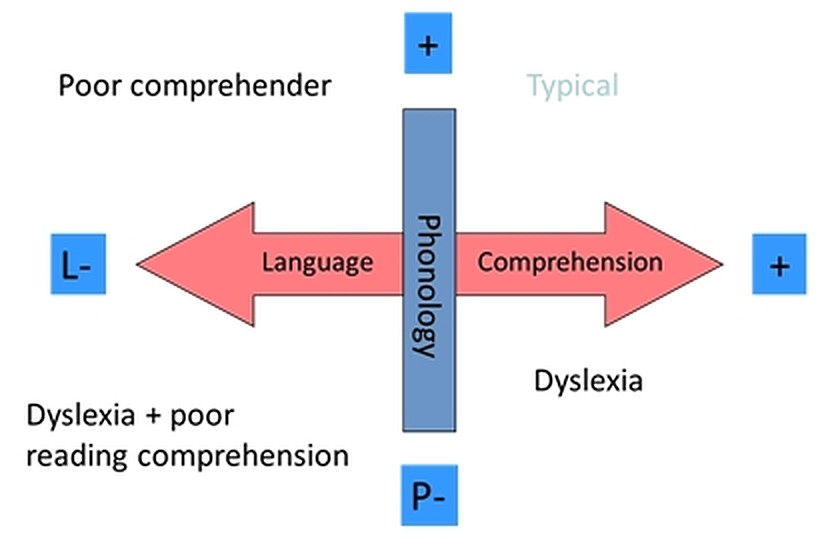
In the diagram above, dyslexics are shown lower down the phonology vertical, while DLD (“poor comprehenders”) are shown horizontally on the left of the language comprehension spectrum. The bottom left quadrant are the combined dyslexics with poor listening skills, and DLD with poor reading comprehension.
Recent studies have shown that dyslexia and DLD are indeed two distinct separate entities, but they frequently share comorbid impairments.
Epidemiology
The prevalence of dyslexia ranges from 7% to 15%, with an average of about 10%, while the prevalence of DMD is slightly lower at 7% (4). Dyslexia is the commonest learning problem.

Epidemiological studies (5) show a male predominance ranging from 1.5:1 to 3.3:1. There have been some comments that perhaps females are underdiagnosed because they are less frequently referred to diagnosticians. The reason why males are more frequently finger-pointed and referred, is because dyslexic males tend to have more unruly behaviour and express their frustrations more physically in class. This male-female inequality is still being studied and debated.
Early Diagnosis (6)
It is unusual to diagnose dyslexia under the age of 1 year. Most children are diagnosed after the age of 2 years. One suspects the diagnosis when the child learns new words slowly, takes longer learning how to speak, finds rhyming challenging, are unable to distinguish between different word sounds, reversing sounds in words, or confusing words that sound alike. At nursery school or kindergarten they may display difficulty spelling, avoid activities that involve reading, spend a long time to complete reading or writing-related tasks, read below the level expected of their age, have difficulty copying from a book or a board, have difficulty remembering or understanding what they hear, are unable to pronounce unfamiliar words, or have difficulty finding words to express their thoughts.
Let’s step back for a moment. Any child who is slow with language development must first have their hearing checked. It would be sad to miss the diagnosis of hearing impairment, as the treatment is totally different from that of dyslexia.
The British Dyslexia Association lists the following early signs that should raise your suspicion of the diagnosis of dyslexia (7):
Genetic Causes (8,9)
Dyslexia often runs in families, suggesting that there is a genetic component, and indeed this is by far the commonest cause. However, some people develop dyslexia after a brain injury arising from infection, trauma, or a stroke. But these “environmental” causes are relatively rare.
Deletion of the DCDC2 gene is associated with difficulty detecting certain types of visual movements (1). Mutation in the ROBO1 gene link between auditory pathway to the brain is weakened (12). These, and many more gene mutations, are believed to converge to cause dyslexia.
The importance of studying genes is that they control protein synthesis and neural connections, among its many functions. Hence further research into this area can provide further insights into the pathophysiology of dyslexia.
Brain Imaging Studies (12,13)
Functional MRI Scans the whole brain and shows the connectivity between different regions. Weaker connections in certain parts of the brain correlate with dyslexia. Brain imaging studies have shown that there are differences in how the dyslexic brain is structured and how it functions.
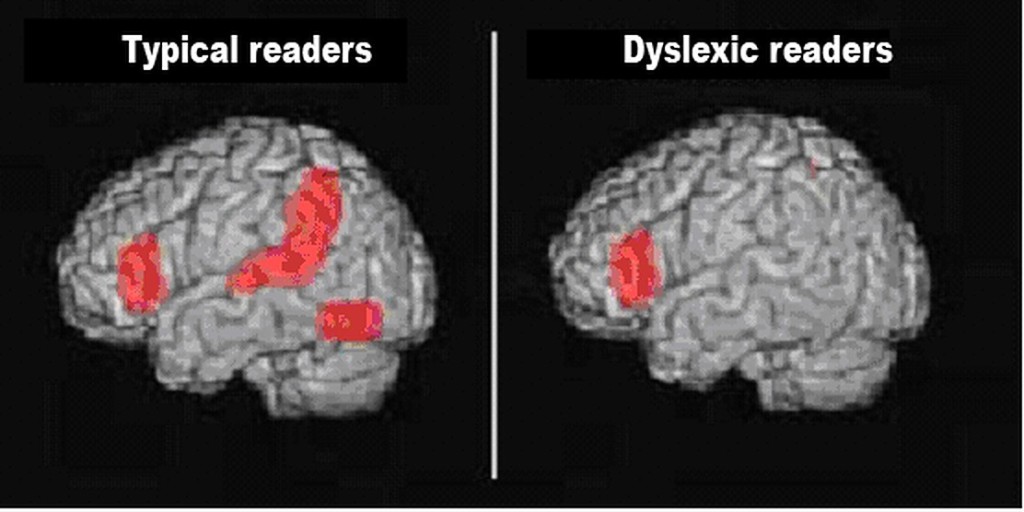
There are no problems with vision, or motor coordination. (See the references for more detailed analyses).
Controversy: Phonological Deficit Hypothesis (14)
Is dyslexia a problem of hearing, reading, or understanding language? In other words is it an auditory problem, a visual problem, or a problem of making sense of words? One of the earlier theories of dyslexia is the Phonological Deficit Hypothesis.
The basis of this hypothesis is founded on the observation that reading is a complicated process and starts with recognizing individual words and sounds. Each word can be dissected into smaller sound elements which are known as phonemes. For example the word “cat” can be broken down into 3 phonemes: “kuh”, “aah”, and “tuh”. Dyslexics have problems distinguishing the words into distinct phonemes elements. This makes it difficult for them to match specific sounds to specific letters. Difficulty distinguishing “volcano” to “tornado”. Inability to join sounds to letters results in dyslexia.
The Phonological Deficit Hypothesis has been challenged, and has currently fallen out of favour, However, it formed the basis of one of the therapies used in the management of dyslexia, the Orton-Gillingham Approach (15). This technique is to help break words down into their component sounds, match the sounds to the letters, and then blend those sounds together. This therapy employs a multi-sensory approach. For example, children might be asked to trace letters in sand, or clap out syllables in words. To date there is no convincing evidence that this technique improves dyslexia.
Problems Associated with Dyslexia (16)
Children who have dyslexia have difficulty reading and writing, and take a longer time to understand what they are taught. They tend to do poorly in spelling tests and school exams, which will lower their self-esteem., and some may even become anxious and depressed They are also at increased risk of having impulsive behaviours, attention deficit hyperactivity disorder (ADHD).
The Mayo Clinic lists the following problems if dyslexia is untreated:
Tips for Parents on How to Manage Dyslexia
1. Start reading to your child from a young age. Interest them with picture books and use emotions to represent the different characters of the story. Point to words of interest in the book. Get your child to guess what happens next in the story. Make reading an enjoyable positive experience.
2. In an older child, get them to read back parts of the story to you, gently giving corrective feedback. You can also monitor how long it takes for your child to read a short passage. Children can enjoy being timed, and they take delight in seeing if they can improve their time. Repeating the reading of a passage can improve fluency.
3. Build vocabulary. Ask your child to inform you of the new word they have learned every day. Talk about the word, its meaning, placing the word in a sentence, and checking on its meaning in a dictionary. Play word games where you try to insert the new word into a sentence at least twice that day, then again that week. Write down the daily list of new words and run through them weekly.
4. Play games. Engage your child by playing fun word games. For example, clap with each syllable of a word spoken out loud. Separate the components of a multi-syllabic word, and them join them back together. Point out alliterations (sound duplications) in songs, poems, and nursery rhymes.
5. Sing songs, learn to play music instruments. Many dyslexics display music, artistic, and other creative talents. Encourage them.
6. Go high-tech. Don’t be afraid to use computer resources, apps, digital learning games. Instruction must be explicit, motivating, systematic, and supportive. Be guided by what classroom is also teaching. But do not spend too much time on the computer at home in case your child becomes too addicted to it!
Practical Classroom Management
a) Students learn more effectively in small groups (preferably 1:3 to 1:6) but this may not always be possible to achieve in some schools. Ideally the teachers should have received training in the teaching of children on how to read.
b) Try introducing and talking around the subject matter before reading the text. Whenever possible, relate the text to real life experiences. Enhance the teaching with pictures, common household items, outdoor activities and field trips.
c) Increase vocabulary by selecting practical high-utility words. Apply the new words in conversation and in writing. Teach proper pronunciation by properly reading the words, and learn about word derivations and manipulations (roots, affixes). If the word has several meanings when used in different contexts, talk about them. Explore figures of speech, synonyms and homophones, and try to give concrete applications of these words.
d) Teach the rules of language, correct spelling and the exceptions where the rules are allowed to be broken.
e) Get the child to read texts pitched at their level. Use the same words in different contexts, and try fluency drills with repeat practising of these same words.
Bilingualism (17)
Many schools advise parents and caregivers of dyslexic children to avoid bilingual language use at home. Research evidence does not show any advantages or disadvantages of dyslexics from bilingual families. Certainly bilingualism is not a cause of dyslexia. Converting into monolingual conversations at home also shows no benefit. Some have suggested that bilingualism might even benefit dyslexics learning to read, but there is no evidence to support this claim either (17).
Different Languages and Different Countries (18,19)
What is fascinating is the comparison of the prevalence of dyslexia in different countries :

Fig 1. Percentage of dyslexics according to corresponding countries (Husni, Jamaluddin 2008) (18)
However, studies like this have been subject to criticisms. The different prevalence in different countries may be due to a combination of other factors, including different cultural and socioeconomic environments.
Another comparison (20) is showing that the prevalence of dyslexia in China is 3.9%, which is lower than the prevalence in western countries, which range from 5 to 17%. But before you draw the conclusion that pictographic languages like Chinese are less likely to result in dyslexia, studies of Japanese dyslexics come to the opposite conclusion. The difference between dyslexics in hiragana, the Japanese alphabet is very low, at 1%. In contrast, the prevalence of dyslexics using the kanji pictorgram is higher at 5-6%.
Below is a mouse, used in English, and a similar-sounding word in several European languages. The captions under the picture show how other languages write the equivalent of mouse in their own native writing. There must be a range of difficulty in reading and writing these different languages. Researching the mechanisms of language learning is important in getting into the fundamental understanding of brain function. Another area of suggested research is to see how different languages can affect the behaviours and personalities of the native speakers. And another area of research is to compare computer language with human language, and how artificial intelligence can merge the two together.

New Technology (21)
There are many new ways to help dyslexics, and the number of new devices and programs are increasing. Here are some that are currently available.
1 Dragon Naturally Speaking transcribes spoken into written words, and translate the words into other languages.
2 Natural Reader is the opposite of Dragon Naturally Speaking, in that it converts the written text into speech. It also has an inbuilt translator so that the speech can be delivered in another language.
3 Livescribe Smart Pen facilitates writing on a computer, and has other functions including audio recording.
4 New fonts with alphabets designed to be heavier at the bottom, so as to prevent readers turning the alphabet upside down.
5 Functional Magnetic Resonance Imaging (fMRI) can observe in real time which areas of the brain are used in speech and reading. This enables one to diagnose dyslexia, as well as to assess which therapy is most effective in training the dyslexic brain to speak, read and write.
Early History of Dyslexia (22)
Doctors and medical students will remember the name Adolph Kussmaul, who described the slow sighing breathing in diabetic ketoacidosis, and is now known as Kussmaul respiration. In 1877 he coined the term “word-blindness” to describe patients who had difficulty reading. Ten years later, in 1887, a German ophthalmologist, Rudolf Berlin, first used the term “dyslexia” to describe the patients who despite having good eyesight, was unable to read the written words. In 1896, the British physician first identified the condition in a child, and describedthe symptoms of dyslexia in greater detail.
Famous Dyslexics (23)
The list of famous dyslexics is very long. We suspect, but cannot prove whether those famous people who are no longer with us, really did have dyslexia. But we do have some reasons why we think Leonardo da Vinci had dyslexia. Although none of these findings are diagnostic by themselves, the combination leads one to think he was dyslexic. He drew and wrote with his left hand, he was able to write mirror image effortlessly (a feature of many dyslexics), and he frequently made spelling mistakes especially in homophonic words.
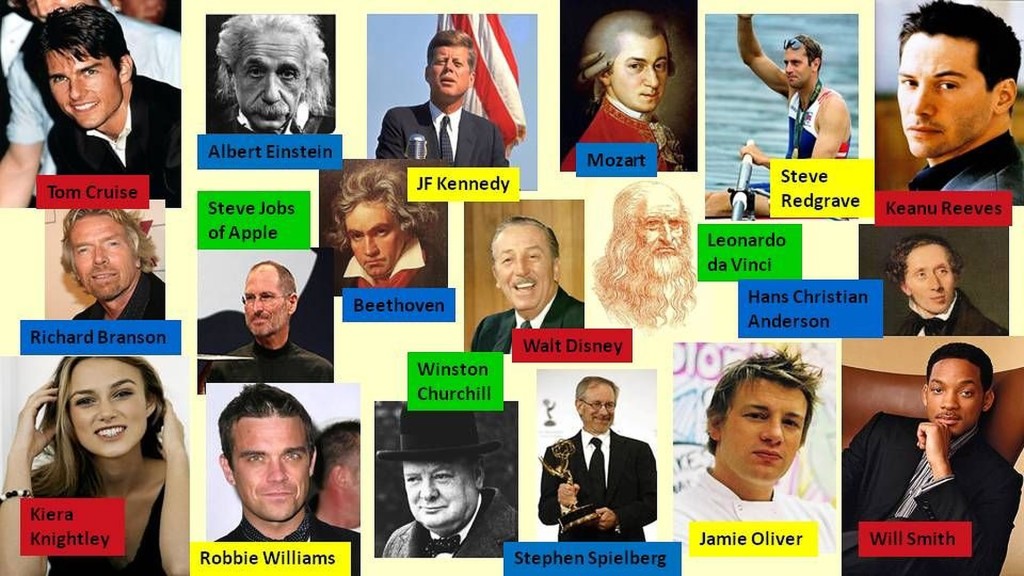
It is also interesting to note that 35% of entrepreneurs are dyslexic, compared to 10% of the general population. These dyslexic entrepreneurs appear to be good at creating new ideas, they are often good at speaking and delegating tasks.
The question all of us are asking is why so many world-famous brilliant people dyslexic? One would have thought that the inability to read and write fluently must be a handicap. So why have so many people accomplished such incredible strokes of genius?
One popular theory is that if you are handicapped in one area, you will overcome the difficulty by finding another area to excel in. For example, the blind can hear sounds and touch objects more sensitively, and the deaf and see more clearly. What seems quite counter-intuitive are the famous writers, some of them confessing that they do suffer from dyslexia.
Conclusions
Dyslexia is a common condition affecting around 10% of the general population. Early recognition can help the affected person become more fluent in reading, writing and understanding language. This will have psychological benefits. Researching into the mechanisms of dyslexia, an the different forms it takes in different languages and cultures can help deepen one’s understanding of how we acquire knowledge and communicate with one another. Hopefully we will gain insights into how we think, and how we develop our personality.
References
1 International Dyslexia Association. Definition of Dyslexia.
https://dyslexiaida.org/definition-of-dyslexia/
2 Catts HW et al. Are Specific Language Impairment and Dyslexia Distinct Disorders?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2853030/
3 Snowling M. Dyslexia and developmental language disorder: same or different?
https://www.acamh.org/blog/dyslexia-developmental-language-disorder-different/
4 Laasonen M et al. Understanding developmental language disorder
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5963016/
5 Arnett AB et al. Explaining the Sex Difference in Dyslexia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5438271/
6 Yale Center for Dyslexia and Creativity. Suspect dyslexia? Act early.
https://dyslexia.yale.edu/resources/parents/what-parents-can-do/suspect-dyslexia-act-early/
7 British Dyslexia Association. Signs of dyslexia, early years.
https://www.bdadyslexia.org.uk/advice/children/is-my-child-dyslexic/signs-of-dyslexia-early-years
8 Hensler BS et al. Behavioral Genetic Approach to the Study of Dyslexia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2952936/
9 Schumacher J et al. Genetics of dyslexia: the evolving landscape.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2597981a
10 Chen Y et al. DCDC2 gene polymorphisms are associated with developmental dyslexia in Chinese Uyghur children.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5361510/
11 Hannula-Juppi K et al. The Axon Guidance Receptor Gene ROBO1 Is a Candidate Gene for Developmental Dyslexia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1270007/
12 International Dyslexia Association. Dyslexia and the brain.
13 Elnakib A et al. Magnetic resonance imaging findings for dyslexia.
14 Wikipedia. Phonological deficit hypothesis
https://en.wikipedia.org/wiki/Phonological_deficit_hypothesis
15 Wikipedia. Orton-Gillingham.
https://en.wikipedia.org/wiki/Orton-Gillingham
16 Mayo Clinic. Dyslexia
https://www.mayoclinic.org/diseases-conditions/dyslexia/symptoms-causes/syc-20353552#
17 Rosen P. FAQs about bilingualism and dyslexia.
https://www.understood.org/en/learning-thinking-differences/child-learning-disabilities/dyslexia/faqs-about-bilingualism-and-dyslexia
18 Husni H, Jamaluddin Z. A retrospective and future look at speech recognition applications in assisting children with reading disabilities.
Click to access Husniza_husni_WCECS2008_pp555-558.pdf
19 Butterworth B, Tang J. Dyslexia has a language barrier.
https://www.theguardian.com/education/2004/sep/23/research.highereducation2
20 Sun Z et al. Prevalence and associated risk factors of dyslexic children in a middle-sized city of China.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0056688
21 Nixon G. How technology Is changing treatments for dyslexia.
https://www.gemmlearning.com/blog/dyslexia/technology-is-changing-treatments-for-dyslexia/
22. The history of dyslexia.
https://dyslexiahistory.web.ox.ac.uk/brief-history-dyslexia
23. List of dyslexic achievers.
https://www.dyslexia.com/about-dyslexia/dyslexic-achievers/all-achiever
Written by Kenneth Lyen
22 June 2021

by Kenneth Lyen
Special Education
Upon returning to Singapore from his post-graduate studies in Philadelphia (1983), Dr Kenneth Lyen joined the Department of Paediatrics at the National University of Singapore. He was soon asked by Professor Freda Paul who was about to retire, to take over her Clinic for the Mentally Disabled, a clinic that took care of over 1,000 intellectually and physically challenged patients. When he took charge of this clinic he quickly realised that there was a gap in the services in Singapore. There were no educational or rehabilitation therapies for children under the age of 7 years which amounted to over a couple of hundred of his patients. “We better do something for them!” he told his colleagues.
A proposal was made in 1985 to Dr Ee Peng Liang, then President of the Singapore Council of Social Service and Community Chest, to start a special school for children under the age of 7 years, who were intellectually and physically challenged. Soon, a vacant school site at Margaret Drive was allocated by the Dr Tay Eng Soon, the Minister of State for Education, to establish special education at the Margaret Drive Special School (now known as Rainbow Centre Margaret Drive School). In 1987, the school was officially opened, launching the Programme for Children with Multiple Handicaps and the Early Intervention Programme for Infants and Young Children (EIPIC) which was started at the Singapore Association of Retarded Children (now renamed Movement for the Intellectually Disabled of Singapore (MINDS).
The First Programme for Children with Autism in Singapore
Over time, Dr Lyen noticed through his clinician practice that there was a special group of children who had socializing difficulties, speech problems and repetitive behaviours, all pointing toward Autism Spectrum Disorder (ASD). He consulted a psychiatrist who, to his surprise, remarked that there were no children with ASD in Singapore. “That can’t be so,”
He soon realized that the definition of autism used by some Singapore psychiatrist and paediatricians was based on Leo Kanner 1943 definition that required autistic children to have zero speech, no socializing abilities, and extremely obsessional repetitive behaviours. When Dr Lyen reviewed the children attending my Developmental Clinic, he noted that his patients had a milder form of autism, with some speech, some social impairments, and repetitive behaviours, more like the behavioural spectrum described in 1944 by Hans Asperger.
He was able to convince both the Ministry of Education as well as the Ministry of Community Development that to start a new special programme devoted to helping children on the autistic spectrum. This was approved in 1987, and once again Dr Lyen approached Dr Ee Peng Liang of the Community Chest to provide funding, which he gave unreservedly.
Structured Teaching for Exceptional Pupils and the TEACCH Programme
In a stroke of perfect timing, renowned clinical psychologist Dr Vera Bernard, who had a special interest in ASD visited Singapore. She approached Dr Lyen in 1988, wondering if she could help in any way. He accepted, and this eventually led to the launch of Rainbow Centre’s Structured Teaching for Exceptional Pupils (STEP) for children with autism ages 2 to 12, a first among Singapore special schools. This was officially started in 1989.
Dr Bernard was invited to the Margaret Drive Special School, and she explained that she would use behaviour modification as the mainstay of the program. She had worked under Professor Bernard Rimland at the University of California San Diego. The STEP program that Dr Bernard was introducing to Singapore was largely based on the Treatment and Education of Autistic and Related Communication Handicapped Children (TEACCH). This was developed at the University of North Carolina, originating in a child research project begun in 1964 by Eric Schopler and Robert Reichler.
The highlight of this program was that therapy was individualized, a philosophy which the Rainbow Centre had embraced when it started the Early Intervention Program. Another aspect of the TEACCH program is that it has a structured format developing the child’s individual potential skills, including visual, auditory, physical, and other abilities. It also recruited parents or other caregivers to learn and become involved in the training using positive behavioural reinforcements, and not aversives.
Over time, the students that attended TEACCH learnt to speak, socialize better, and their obsessional behaviors diminished, compared to those children on the waiting list.
Executive Director
An executive director was recruited to manage the school as well as the new STEP program. June Tham was head-hunted and invited to join the Margaret Drive Special School. Initially she did not want to leave her position in another special school, but in 1989 she agreed to become the executive director of the school.
The Rainbow Cenrtre
The STEP was started with 12 students. Since then the numbers has progressively increased to the current number of over 700. The Margaret Drive School was soon unable to cope with the increasing number of students, and a second school was started in 1992 which is now located at Yishun Park. Both schools took in younger children under the age of 12 years on the autism spectrum. To manage two schools, an umbrella body, the Rainbow Centre was officially established in 1992. In 2018, another school, the Woodlands Campus was started, making it the third school under the Rainbow Centre.
In 2004, some members of the Rainbow Centre were approached by the Ministry of Education to help start a school for autism spectrum children above the age of 7 years. Several Rainbow Centre board members volunteered to help start the Pathlight School, which was led by Denise Phua. This school served students who were capable of pursuing the Primary School Leaving Examinations (PSLE) and the General Certificate of Education (GCE) exams. An additional education track was started for those suitable for vocational skill certifications. Pathlight School launched the Satellite School Model in 2005 in which its secondary schools students were physically located with their teachers in several partner mainstream secondary schools such as Chong Boon Secondary School and Bishan Park Secondary School; for fuller social and academic integration.
Other Schools
There are now many more schools in Singapore handling children with autism spectrum disorders, including Grace Orchard, Eden School, St Andrew’s Autism Centre, and the older schools of MINDS and Association for Persons with Special Needs (APSN) also take in autistic students. There is now an autism resource centre, as well as several centres that organize co-curricular activities. As for the older persons with autism spectrum, there are now job-training programs, helping them find employment in the food and beverage industry, gardening, working in an office, and computing.
Singapore has recognized that there are children within main stream school settings whose special needs require additional support beyond what is usually available in schools. Services supporting such students, particularly those with mild dis abilities, have been steadily developing. However, the 21st century has seen great leaps in services for children with special needs, in line with the government’s focus on making Singapore a more inclusive society.
In the sections that follow, we will describe two developments in mainstream schools since the 1970s, as well as other organisations supporting special needs students who are attending them.
In 1970, the Ministry of Education established the Schools Social Work and School
Psychological Services, and this was later renamed as the Psychological Services Branch. Staffed by educational and associate psychologists, the aim was to provide support to students with special needs in mainstream primary schools. This branch also provides support to the Allied Educators (Learning and Behavioral Support) (AED [LBS]).
Another initiative to provide early intervention to students who required support in their acquisition of literacy skills was started under The Learning Support Programme (LSP) was introduced in 1992. This was subsequently expanded in 1999 to provide the same screening and support for students who are weak in mathematics.
Currently all trainee teachers must receive a 12 to 36-hour introductory course on special education to help accommodate and support students with learning difficulties.In addition, 10% of primary and 20% of secondary school teachers receive over 100 hours of training to further assist students with special needs in mainstream settings.
Fundraising
As the school population grew, the existing facilities were unable to support the students’ needs. When the time came for a new purpose-built building, the team embarked on fundraising initiatives. As a member of the Rotary Club of Singapore North, Dr Lyen took up the mantle for fundraising. Support was also given by other charity bodies like the Lions Club, The Lee Foundation, the Tsao Foundation, and many other bodies.
Future Challenges
The hopes for the future:
The first is to adopt a lifespan philosophy that looks at the entire life of a person on the autism spectrum This requires more training, more jobs, more support. The next problem is to find ways of looking after those on the more severe end of the spectrum, especially when their parents and loved ones pass on. Who will look after them?
The second challenge is raised by the higher functioning autistic individuals. They do wished to be labelled “disabled”, but to be regarded as “differently abled”. In other words they do not want autism to be regarded as an abnormality or a pathological disease. They want to be seen as merely different. One repercussion of this is that mainstream schools need to be able to become inclusive and allow everyone of different abilities, to study together, to play together, and to be considered as part of humanity’s one big family. This is already taking place in nursery and kindergartens. Many of them are accommodating children on the autism spectrum. Hopefully this will extend to older agegroups.
Inclusive education: Different, not disabled. I do not believe in segregating children with differences into separate schools or institutions. Children have different abilities and interests, but we should not partition them into isolated schools. They can still join in other activities such as sports, art, music, dance, etc. We need to develop a mindset that we are all part of a family
Prevention is better than cure. If we can discover the causes of childhood developmental conditions, we may be able to prevent more of these states. Already the incidence of Down Syndrome and cerebral palsy has fallen. I hope that autism will follow suit.
New technologies. Creating new technologies to help the disabled should be given more funding. Enhancing communication, facilitating the integration of special children into society, allowing them to travel, shop, etc with ease can be developed further.
These are our hopes for the future.
Acknowledgment
The section on Mainstream Schools was written by Kenneth Poon
References
June Tham (ed) Rainbow Dreams
https://www.amazon.sg/Rainbow-Dreams-Kenneth-Pathnapuram-Tham-Toh/dp/9814413631

by Kenneth Lyen
INTRODUCTION
Just as there is a spectrum of autistic individuals, there is also a spectrum of families into which they belong. Some families are thrown out of balance when they are challenged with a child who needs extra support and management. Others cope with the myriad of difficulties with self-assurance. Here we will focus on the more severe end of the autistic spectrum that poses stresses upon their families. What are the challenges facing them?
COPING WITH AN AUTISTIC FAMILY MEMBER
1. Challenge: How to come to terms with the diagnosis?
Approach: It can come as a shock to learn that your child has autism. None of us are prepared for this. And we will go through a wide range of emotions ranging from fear to anxiety and despair. We love our child so much, and we want to give them the very best in life, but now we fear the worst, our hearts suffering agonizing pain. Initially you may deny the diagnosis, and later you might become angry and even depressed, before finally you begin to accept the diagnosis. Some of your friends may try to convince you that autism is not a disease, but just a different condition, that will sort itself out in the end. But this will probably not help your grief.
It is important to try to obtain more information, either through online sites, books, or talking to recognized teachers, psychologists or medical specialists about the diagnosis. Given the characteristics of autism, it is important that you and your family seek professional advice early, as this can help you learn how to engage and connect with your child, and to become more flexible and understanding of your child’s behaviours, feelings, and development.
2. Challenge: How would you deal your other family members’ reactions to the diagnosis?
Approach: You may have begun to accept the diagnosis of your child, but then you have to inform other members of your family. Each one will probably respond differently. Perhaps you might want to talk to each member separately, including your spouse, your siblings, grandparents, and other caregivers. The reason is that autism is a lifelong condition that requires teamwork and long-term management. This can only come about when everybody accepts and understands the condition and learns how to work together to cope.
Having a child with autism can be very lonely for you. It is not uncommon for parents to keep the child’s diagnosis hidden from their immediate family and even their friends and colleagues. It is probably better not to conceal your child’s condition from others, because eventually you will need to enlist the help of your friends, neighbours and other members of the community.
3. Challenge: How should we accept our autistic child?
Approach: Accept your child as they are. Accept their idiosyncracies, their unusual mannerisms, their quirks. There are times they will be exasperating, like crying for long periods, and nothing you do will stop the crying. Don’t give up. Engage with them, love them. Children will grow up and change with time. You too will learn to adapt.
4. Challenge: How should we change the physical environment of our home?
Approach: Autistic children are sensitive to the environment. First, the home environment should be safe. Avoid getting furniture with sharp corners. Keep dangerous implements away. Cover electric sockets with electric plug protectors. Construct window grills to prevent the child jumping out of the flat.
Reduce noise because many autistic individuals have sensitive hearing and cannot stand loud noise. This also applies to television, radio, and home cinemas. Same treatment with bright lights. Many autistic people do not tolerate lights that are too glaring.
Have a variety of safe toys. Some autistic children like to line up objects, like cars, so perhaps one should not buy too many similar vehicles.
5. Challenge: Should we set a timetable?
Approach: Yes, autistic children learn and develop better with a predictable programme. You should set up a detailed structured schedule that can be followed every day. This includes waking up at around the same time, brushing teeth, washing face, toileting, changing clothes, having breakfast, playtime, exercise time, etc, all the way to bedtime.
6. Challenge: How should we communicate with our child?
Approach: Some autistic children may have delayed speech, and some remain silent for much of their lives. Look out for nonverbal cues. Look at their facial expressions to determine their mood. Look out for body language, their gestures, their responses to food, toys, and other activities. If they are not looking at you, turn the head to look at your face. Use a combination of visual and auditory clues to communicate, supplemented by your supplying the words to describe the activities or objects.
Try not to spend too much time watching television, playing on the mobile phone, or laptop computer. Anecdotal evidence suggests that such activities do not stimulate communication or speech.
7. Challenge: How to optimize learning?
Approach: Find out their strengths and weaknesses. What do they enjoy? Do they enjoy certain activities like drawing, playing the piano, or constructing objects with Lego? Make playtime fun, but cap the time devoted to any particular activity, so it does not become obsessional.
8. Challenge: How to tackle undesired behaviours?
Approach: Some autistic children indulge in prolonged repetitive behaviours, like clapping, flapping hands, rocking, and even self-injurious activities. They may make unusually loud noises, or scream continuously. One approach is to distract them and try to persuade them to take part in another activity or play with another toy. Try to discover if there may be some recognizable triggers for these behaviours. For example, is it in response to your refusal to give them what they want? Maybe you do not realise what they really want, and they are unable to express themselves in words. So in frustration they start screaming.
In the case of self-injurious or dangerous behaviours like head-banging, biting, pushing, or scratching, you need to stop these activities immediately. If necessary, make an appointment to consult a doctor.
9. Challenge: Should we engage in special therapies
Approach: The special therapies referred to include speech and communication therapy, occupational therapy, physiotherapy, music and art therapy. Most special schools, nurseries and kindergartens with interest in autistic children, should be able to provide some of these therapies. When you have identified those areas that you think your child might need extra encouragement and help, then you might like to discuss if they are really beneficial, and where to find these therapies.
10. Challenge: A brief overview of the autistic child’s future.
Approach: Different stages of the autistic individual’s life will require different approaches. The young autistic child may need early intervention centres that may help in several ways, including giving family support, and providing speech therapy, occupational therapy, and special education. Opportunities for socializing needs to be organized, so the child can mix with other children, be given opportunities to engage in art, music, sports, and outdoor activities. The long-term future may require drawing up a will, and setting aside some funds in the event that the individuals are unable to take care of themselves, especially after the parents have passed on.
11. Challenge: How not to be overwhelmed by too much information on the internet.
Approach: It is a typical response for parents to be overenthusiastic in seeking (too much) information for the sake of their child on the world wide web. The internet is a vast storehouse of information, but unfortunately not all the information is accurate. It is important to check the facts to verify whether they are reliable. Also discuss the data with other professionals to evaluate their accuracy and relevance.
12. Challenge: Strain on marriage
Approach: Looking after an autistic child can be a heavy strain on one’s marriage. Sometimes getting relatives and friends to help out can alleviate the problem. If not, one may have to look for marital or family counseling for help.
13. Challenge: Who would be best to confirm a diagnosis of autism?
Approach: The diagnosis of autism spectrum disorder should be an experienced paediatrician, psychiatrist, or psychologist familiar with autism. A teacher or a general practitioner, or another parent, should also be able to guide you. You can also search the internet for online websites that can lead you to resource centres, special schools, and government websites dealing with autism. These websites might be able to provide information, advice, and direct you to the appropriate psychologists and medical specialists to obtain a diagnosis.
The Autism Resource Centre (ARC) was set up specifically to focus on the education of autism for families and autistic individuals. ARC has also been running Certificate and Diploma in Autism courses for educators from both mainstream and special education institutions. They also run parent training workshops for parents and the public.
14. Challenge: Which pre-schools and schools to choose from?
Approach: There are several factors to consider. This includes which end of the autistic spectrum your child comes under. Are there any co-morbid problems, like attention deficit hyperactivity disorder, epilepsy, aggressive behaviours, etc? How far is the school from where you live, and is transport provided? Best to visit the schools and discuss your child with the teachers, principals and other parents.
15. Challenge: How to find help for low-income families?
Approach: Some children with autism require special education, early intervention, and other therapies, but these can be quite costly. What kind of help is available for low-income families who are raising children with autism? Fortunately, there are government organisations and charitable foundations that can give a helping hand. See the list below.
CONCLUSIONS
Teamwork is the foundation of coping with autism. The good news is that there are now quite a number of organisations, schools, psychological and medical services that can help. The problem is trying to find what would be best for your child and for your family. The internet can overwhelm you with too much information, and the most attractive site may not offer the best advice or therapies. Discuss it with as many people as possible, including teachers, psychologists, doctors, and other parents.
Final advice: Love your child, and don’t give up!
RESOURCES
Singapore Autism Resource Centre. https://www.autism.org.sg/
Singapore Rainbow Centre. https://www.rainbowcentre.org.sg/
Singapore St Andrew’s Autism Centre. https://www.saac.org.sg/
Malaysia Autism Link. https://www.autism.my/
Malacca Malaysia. http://www.wingsmelaka.org.my/
UK National Autistic Society. https://www.autism.org.uk/
Free Online Courses:
http://www.autism-society.org/living-with-autism/how-the-autism-society-can-help/online-courses-and-tutorials/
Floortime DVD Autism Training: https://www.amazon.com/Floortime-DVD-Training-Basics-Communicating/dp/B0009XZITG
Online resources screening tools:
0-2 years – http://asdetect.org/
18 months – Checklist for Autism in Toddlers (CHAT)
https://www.rch.org.au/genmed/clinical_resources/CHecklist_for_Autism_in_Toddlers_CHAT/
4-11 years – childhood Asperger syndrome test (CAST)
https://www.autismresearchcentre.com/project_9_cast

by Kenneth LYen
INTRODUCTION
Autism awareness campaigns have been largely successful – more people know what it is, how to recognise the signs, and diagnosticians are better equipped to identify and properly diagnose the condition. With the worldwide connection on the internet, there is an increasing amount good reliable information. Unfortunately there is a burgeoning amount of false information or “fake news”. These often fuel some people’s strongheld distorted beliefs about autism. Trouble is that it is often difficult to separate truth from lies or partial truths. Below we will sift through some of the prevailing myths about autism, and try to determine which ones we think are true, partially true, or outright wrong.
MYTHS ABOUT AUTISM
1. Myth: People with autism don’t want to make friends. (1)
Answer: In most cases this is untrue. What is true is that they have difficulty making friends as they may not have the repertoire of social or communication skills to be able to do so. However, they can be taught to socialize and communicate. Most persons with autism do want to make friends and can love as deeply as any other person. They form close relationships with people who they are familiar with, such as relatives and caretakers. With time, they bond with their peers, teachers and therapists who they frequently interact with.
2. Myth: People with autism can’t feel or express any emotion—happy or sad. (2)
Answer: It is not that autistic individuals cannot feel or express emotions, but that they do so in a different or less expressive way. They do show a degree of empathy, and can recognize happy or sad faces. But when it comes to more subtle emotions, such as anger, fear or irony, they may have a harder time. Autistic people may have a more muted, less expressive way of displaying their emotions. Some get angry very quickly, while others may misread a situation and respond inappropriately; for example when they see someone fall down, they may laugh because they are not aware that the person may be hurt.
3. Myth: People with autism are intellectually disabled. (3)
Answer: Autistic individuals, like the rest of the general population, have a wide range of abilities. Many have difficulty with speech and language, and this may give the mistaken impression that they are intellectually challenged. When it comes to cognitive abilities, like any other person, there will be autistic subjects with intellectual disability. On the other hand, there are some who display outstanding prowess in mathematics, art, music, and other abilities.
4. Myth: Individuals with autism spectrum disorder cannot lead independent and successful lives. (4)
Answer: This is not necessarily true. Those who are more severely affected with limited language skills may have difficulty navigating our rather complex modern-day society without help. Those on the milder end of the spectrum can learn skills that enable them to get jobs, enter mainstream education, and lead independent lives. Training and special education can be very beneficial for autistic individuals, and this is highly encouraged.
5. Myth: Autism can be cured. (5)
Answer: The majority of autistic persons remain autistic all their life. They can make significant progress with early intervention, special education, and vocational training that has been specially tailored for the needs of each individual. At the moment many medicines have been tried to reduce the manifestations of autism, but to date, none of them are effective. With advances being rapidly made on the causes of autism, it is hoped that one day it may be possible to prevent or cure autism.
6. Myth: Autism is caused by bad parenting. (6)
Answer: The theory that autism is caused by bad parenting, or mothers who lack emotional warmth (“refrigerator mothers”), has been disproven. When parents try to better understand and learn to connect with their children, they can help them flourish.
7. Myth: Autism is caused by vaccines. (7)
Answer: There have been many large-scale epidemiological studies that have shown conclusively that there is no scientific evidence to support any causal link between vaccination and autism.
8. Myth: Autism is caused by food allergies. (8)
Answer: To date, there are some isolated anecdotal evidence that some children’s autistic manifestations seem to worsen with certain foods, such as gluten (wheat), casein (milk), eggs, tomatoes, eggplant, avocado, red peppers, etc. However, there have been no large-scale studies to confirm these data. For the time being, one needs to maintain a healthy skepticism linking autism with food allergies. Thus at this stage, one should not restrict the autistic child’s diet.
9. Myth: Autism is becoming epidemic. (9)
Answer: The prevalence of autism in Singapore is 1 in 150, which is close to the worldwide statistics given by the World Health Organisation. There has been an increase in the number of cases being referred with a diagnosis of autism in the past 30 years, leading to an increase in the numbers diagnosed. In the USA for the year 2000, the prevalence of autism was 1 in 150, but in 2017, the prevalence has more than doubled to 1 in 68. How much of this is a real increase in the number of new cases is controversial. Some experts claim that most of the increase of cases stems from a growing awareness of autism and changes to the diagnostic criteria, especially the Diagnostic and Statistical Manual 5th Edition (DSM-V).
10. Myth: Most autistic individual have special gifts or savant abilities. (10)
Answer: The prevalence of special abilities or savant skills in autistic individuals ranges from 0.5% to 10%. Famous examples include Stephen Wiltshire who has a photographic memory and can draw a city like Singapore after flying over it just once. Temple Grandin is the professor of animal science and a famous author. Kim Peek who has read 12,000 books and remembers everything about them. Leslie Lemke can play the Tchaikovsky piano concerto just listening to it once only. It is postulated that if one has a disability in one area, then the body compensates by developing expertise in another area.
11. Myth: Autism is not a “disease”. (11)
Answer: Is autism a “disease”, a “disability”, a “disorder”, a “condition”, or just a “difference”? The difficulty in trying to see which one of these different terms best fits autism is due to the wide spectrum of this condition. If one takes the severest cases, where the child is profoundly speech delayed, is totally isolated and alone, and flaps their hands or rocks their body endlessly, and continuing intermittently over many years, then it would be amiss of us to downplay the condition by dismissing it being “different”. This does not help the child or family. But at the other end of the spectrum, where autistic individuals can lead a fairly normal life, then it would be fair to say that autism is not a disease. If the problem were purely that of labeling, then it would be politically correct to substitute the word “disease” and consider autism a “disability”, a “disorder”, or a “condition”. As long autism is recognized as a potential problem and that the child and their family gets the help and support they need, then it’s fine to choose whatever term one is comfortable with.
12 Myth: The goal of treatment is to make autistic children “indistinguishable from their peers”. (12)
Answer: Currently, most therapies aim to improve social and communication skills, and reduce the restrictive repetitive movements of autistic individuals. There is a school of thought that suggests that hand-flapping, verbal echoing, and not engaging in social interaction is not pathological, but an adaptive strategy for that person to cope with a world that feels confusing, disordered, uncertain, and overwhelming. The solution is to dig deeper into the reasons for the behaviours, and to modify the environment. For example, if the autistic person is hypersensitive to noise or buzzing fluorescent light, or uncomfortable clothing, then the intervention is to change these environmental factors. There are no right or wrong answers, and probably one can try both paths and see which one works best. Currently most parents choose to modify their autistic child to fit into conventional norms.
13 Myth: We’re just over-diagnosing quirky kids with a trendy disorder. (13)
Answer: When Elon Musk claims to be on the autistic spectrum, or we place the label on Steve Jobs or Woody Allen, many of us raise our eyebrows. Are we too trigger-happy and over-diagnosing autism? Most of us “normal” or “neurotypical” individuals probably have share some autistic symptoms, like having obsessional habits or hobbies, or we may sometimes withdraw into a world of our own, or we cannot tolerate certain people or foods or clothing. So are we over-diagnosing autism especially at the milder end of the spectrum? The problem is that there is no clear cut-off point between normal and mild autism. Until we find an objective blood test or brain scan to confirm the diagnosis, we are likely to over-diagnose mild autism.
14 Myth: Autism is caused entirely by genetics. (14)
Answer: There is certainly strong evidence of the role of genes as a contributing cause of autism. Identical twins have a 70% chance of both being diagnosed with autism. In contrast, non-identical twins only have a 30% chance, and the general population has a less than 2% probability. If genetics were the sole cause of autism, the concordance rate for identical twins should be 100%. The shortfall suggests that another factor must play a role, and the most likely candidate for that is environmental.
15 Myth: Autistics Won’t Get into Higher Education or Get a Good Job. (15)
Answer: At the mild end of the spectrum, some autistic people excel in their studies which qualifies them for higher education. Some of them, like Elon Musk or Satoshi Tajiri who created Pokemon, have succeeded in their enterprise. At the severe end of the autistic spectrum, the poorly communicating, handflapping noisy individual who does not conform to society’s behavioural norms, might well be discriminated against. Currently the unemployment rate of autistic individuals is between 50%-85%. It is hoped that employers will learn to understand and accept the differences of autistic applicants. Also it would be our future hope that society will create more jobs suitable for people on the spectrum.
16 Myth: Only Boys Get Autism (16)
Answer: The ratio of boys to girls on the autism spectrum is 3 to 1. Is it because girls are under-diagnosed? Or is there a real difference in the ratio? If so, the reasons are still unknown.
REFERENCES
1 Denworth L. How people with autism forge friendships.
2 Brewer R, Murphy J. People with autism can read emotions, feel empathy.
3 What are the extremes of intelligence seen on the autism spectrum?
4 Can a person with autism spectrum disorder live an independent adult life?
Can a person with autism spectrum disorder live an independent adult life?
5 What are the treatments for autism?
https://www.webmd.com/brain/autism/understanding-autism-treatment
6 Crowell JA et al. Parenting behavior and the development of children with autism spectrum disorder.
https://www.sciencedirect.com/science/article/pii/S0010440X18301925
7 American Academy of Pediatrics. Vaccine safety: Examine the evidence. https://www.healthychildren.org/English/safety-prevention/immunizations/Pages/Vaccine-Studies-Examine-the-Evidence.aspx
8 Inserro A. Is There a Link Between Autism, Food Allergies? Study Offers Hint But No Answers. https://www.ajmc.com/view/is-there-a-link-between-autism-food-allergies-study-offers-hint-but-no-answers
9 Hess P. Apparent new rise in autism may not reflect true prevalence.
10 Treffert DA. The savant syndrome: an extraordinary condition. A synopsis: past, present, future. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2677584/
11 Stevenson N. Autism doesn’t have to be viewed as a disability or disorder.
12 Brennan D. Parenting a child with autism.
https://www.webmd.com/brain/autism/children-with-autism-coping-skills-for-parents
13 Healthline. Are we overdiagnosing autism?
14 Mundell EJ. Autism Largely Caused by Genetics, Not Environment.
15 Autism Recovery Network. Why is the autistic unemployment rate so high?
16 Loomes R et al. What Is the Male-to-Female Ratio in Autism Spectrum Disorder? A Systematic Review and Meta-Analysis
https://www.sciencedirect.com/science/article/abs/pii/S0890856717301521
17 American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.)
You must be logged in to post a comment.