
by Kenneth Lyen
Rise in Suicides
Today I learnt that one of my student’s close friend had committed suicide. And only a few months ago, one of my colleague’s son had also committed suicide. It is devastating for these families when their young ones, in their early 20s, end their lives.
The Straits Time of the 8 July reported that there were 452 suicides in Singapore in 2020 (1), and the Malay Mail of 29 June stated that in the first quarter of 2021 there were 631 suicides in Malaysia, far higher than in previous years (2). Why do people take their own lives? Is the increase in suicide rates related to the Covid-19 pandemic? I will discuss this later. But first I will examine depression.
What is Depression? (3,4)
It is a feeling of sadness that is felt more intensely and lasts longer than the transient heartaches, disappointments and blues that we all encounter in our daily lives.
Clinical Presentation
There’s a difference between “having depression” and “feeling sad”. We all feel very despondent when we fail an exam, get rejected by an institution of tertiary education, or lose our job. We feel sad, but after a while, we pull ourselves together and overcome this temporary unhappiness. In contrast, clinical depression lingers on for much longer, sometimes two weeks or more. It interferes significantly with our studying, working, playing, eating and sleeping.
Symptoms of depression
The following symptoms are listed in the American Psychiatric Association’s Diagnostic and Statistical Manual 5th Edition (DSM-V) (5):
- Low mood, feeling sad most of the day, occurring nearly every day
- Loss of interest in things one normally enjoy
- Changes in appetite leading to significant weight loss or gain
- Feeling restless, agitated, pacing up and down, psychomotor impairment like slowing of thoughts and movements
- Extreme fatigue, loss of energy
- Feeling of worthlessness or excessive guilt
- Poor concentration, lowered ability to think or pay attention
- Inability to sleep, or oversleeping
- Recurrent thoughts of suicide or have attempted suicide
Diagnosis
According to the DSM-V, you need five or more of the above symptoms to qualify for a diagnosis of depression, On top of that, there are the following additional requirements: these symptoms must cause significant distress to one’s daily life. They cannot be due to the consumption of medicines known to be associated with depression. One needs to exclude substance abuse, and other medical or mental conditions, such as a schizoaffective disorder. There cannot be a manic or hypomanic episode at any point.
Depression can affect men and women all the way from early childhood to old age. No socioeconomic status or ethnic groups are exempt from depression.
Other Symptoms Associated with Depression
We have listed above the official DSM-V symptoms of depression, but most people who have been working with individuals who suffer from this condition are aware of other symptoms listed below, and they should be looked out for:
- Irritability and anger
- Memory loss
- Self-blame
- Brooding and rumination
- Social withdrawal
- Blunted circadian rhythm where the timing of the sleep-wake cycle is disturbed
How Depression Affects One’s Daily Life
There are many ways in which depression can affect one’s daily life. These include:
- Hampering academic studies or work performance
- Disrupting meaningful relationships with others
- Slowing down in getting things done
- Eating a poor diet and becoming malnourished
Depression in Children
Depression in children is quite difficult to pick up, and the diagnosis is often delayed or missed. Symptoms may not be constant, and can fluctuate from day to day, depending on the environment and events. As a child grows up, the manifestations of depression can unfold differently at different ages. One must have a high index of suspicion if a child has continuous feelings of sadness or hopelessness, if there are bouts of anger or crankiness, if they become socially withdrawn, display changes in appetite or food preferences, change their sleep patterns, have difficulty concentrating on schoolwork, cry a lot, or have thoughts of suicide. Some may even present with superficially unrelated symptoms like headaches and abdominal pain, so caregivers and doctors should be alert to the possibility of an underlying depression.
Subtypes of Depression
a) Peripartum Depression
Post-partum depression or “Baby Blues” usually occurs after childbirth, but studies have shown that some mothers may have depression prior to childbirth. Thus, the condition has been renamed “depressive disorder with peripartum onset”. It can occur during pregnancy or up to 4 weeks after birth. Some 10-15% of mothers experience postpartum depression. Symptoms include mood swings, frequent crying, trouble bonding with the baby, tiredness, a fear that they will not be a good mother, or a sense of worthlessness or shame. In women, several hormones including estrogen, progesterone, prolactin and cortisol all decrease significantly after childbirth, and this drop may be responsible for causing the depression. Lifestyle changes may also play a role, because men can also experience depression around the same time. In men, their levels of testosterone and vasopressin fluctuate during and immediately after their female partner’s pregnancy, but the precise mechanism of depression in males is still unclear. Both males and females will experience environmental changes such as dealing with an unconsolable baby, sleep deprivation, changes in one’s daily routines, and having difficulty finding adequate support to take care of baby.
b) Atypical Depression
Atypical depression is characterised by increased sensitivity and reactions to changes in the environment. There may be improved mood during positive events, and this is referred to as “mood reactivity”. This contrasts with “melancholic depression” where even previously pleasurable events do not elevate one’s moods. Atypical depression may exhibit increased appetite, weight gain, heavy feeling in the limbs (leaden paralysis), oversleeping, and and becoming extremely anxious when being scolded or rejected.
c) Persistent Depressive Disorder (Dysthymia)
This subtype is a chronic form of depression which lasts over longer periods of time usually more than 2 years. The severity can also fluctuate over time. Symptoms include changes in appetite, changes in sleep, fatigue or low energy, reduced self-esteem, reduced concentration, struggling to make decisions, feeling hopeless, and harbouring pessimistic thoughts.
Differential Diagnosis
Bipolar Disorder (6)
Bipolar disorder was formerly known as manic-depression, and is characterised by extreme mood swings between hyperexcitable behaviour followed by depression. Some patients are misdiagnosed as suffering from depression. One should try to find out if the person has up and down mood swings, and if there are manic episodes, then this points towards a diagnosis of bipolar disorder. The reason why it is important to make a correct diagnosis is that the treatment differs from depression. Lithium carbonate is the preferred treatment for bipolar disorder.
Seasonal Affective Disorder (SAD)
Depression that occurs either in the winter months or during spring-summer months are diagnosed as Seasonal Affective Disorder (SAD). In those countries where the winter months are cold and the sun sets early resulting in dark afternoons and evenings, can make some people feel rather moody and, as the acronym suggests, sad. It has recently been realised that there is also depression that can occur during the spring and summer months. It is thought that this form of depression is due to allergy to pollen.
Causes (7,8)
The causes of depression are still not fully worked out. There have been a lot of research being conducted utilising advanced technology, and the results are still coming in.
Genetics (9)
If a first degree relative has depression, then one has a higher risk of getting depression too. If an identical twin has depression, the other twin has a 60-80% chance of developing it. A non-identical twin, on the other hand only has a 20% chance of experiencing depression.
The vast majority of individuals suffering from depression do not have close relatives with this condition. Because depression is a heterogeneous condition often overlapping with other personality, behavioural and psychiatric disorders, and there are no laboratory or imaging techniques to make a definitive diagnosis, there is a problem. Is depression a single disease, or is it made up of several diseases with some common and some overlapping symptoms? Therefore, what exactly can one correlate any particular set of candidate genes with?
Unlike other major psychiatric disorders like autism, genetic studies have not achieved very promising results. Following the successful human genome project, where the entire human DNA was mapped out in 2003, several Genome Wide Associations Study (GWAS) have been conducted in many countries, using large sets of samples, including thousands of patients with different forms of depression, and meta-analyses of thousands of patients scrutinised. Unfortunately, all have failed to identify any specific gene loci responsible for the predisposition to depression.
Recently there have been some suggestions that perhaps mitochondrial dysfunction may play a role in the development of major depressive disorders. If true, this throws a spanner in the works!
Environmental Factors
Life Events
Tragic events, like the death of a family member, failing an exam, losing a job, getting divorced, can increase the chances of having depression. A traumatic childhood, sexual or psychological abuse, neglect, poverty, and unhealthy lifestyles, can also predispose one to develop depression later in life. The side effects of certain medicines, like corticosteroids, beta-blockers, and statins (treatment of high cholesterol levels), can result in depression. Recreational drugs, like amphetamines, can also lead to depression.
Based on a combination of genetic and environmental factors, it is postulated that depression has neurochemical and neurostructural aetiologies.
Neuropathology of Depression (10)
The commonest theory about the cause of depression is the theory of chemical imbalance in the brain, especially the lack of serotonin, the “feel good chemical”. This is based on the observation that raising the level of serotonin through medicines can alleviate symptoms of depression in some patients. However, this view does not really capture the complexity of depression.
a) Monoamine deficiency theory
The underlying basis of depression is low levels of serotonin, noradrenaline or dopamine, the monoamines. Each may have an impact on separate sets of symptoms:
- Serotonin: obsessions and compulsions
- Noradrenaline: anxiety and attention
- Dopamine: attention, motivation and pleasure
If one of these monoamine neurotransmitters is down, it may lead to a specific set of symptoms felt by the patient.
Serotonin is thought to be a major player, and perhaps even regulating the other neurotransmitter systems.
Tryptophan depletion: this is the amino acid which the body uses to make proteins including serotonin. Its depletion can lead to symptoms of depression. It also links to DNA studies of depression.
b) Neural Growth and Connections Theory
In recent years, scientists have discovered that brain cell growth and connections may play a larger role in the cause of depression. The hippocampus tends to be much smaller in depressed patients. The hippocampus is the area of the brain that controls memories and emotions. The longer the person has been depressed, the smaller the hippocampus becomes. Stress may be the main trigger to decrease the number of new neurons in this area of the brain. When this area of the brain regenerates and new neurons are stimulated, the mood improves. Many drugs include those that affect serotonin levels, have an indirect effect on the growth of brain cells. Cells that secrete serotonin also secrete other chemicals that stimulate growth of new neurons or neurogenesis.
Investigations
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging shows structural changes in the brain, and this has shown that a part of the prefrontal cortex known as the ventromedial cortex is much smaller in depressed individuals. The ventromedial cortex enables an individual to be stimulated by positive rewards and experience pleasure. It also enables one to switch from one mood to another mood. The cells involved in this function are the glial cells which supplied nerve cells with energy, and the number of these cells is decreased.
Positron Emission Tomography (PET) Scan
Function Magnetic Resonance Imaging (fMRI)
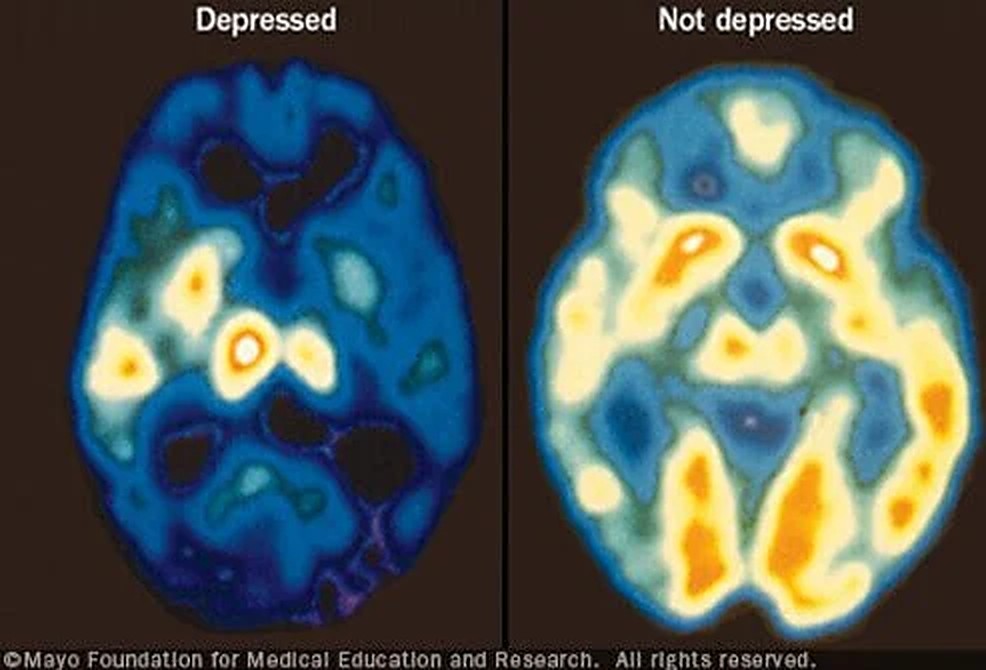
Positron Emission Tomography (PET) Scan allows scientists to determine the metabolic rates of the brain by measuring oxygen and blood sugar (glucose) utilization. Findings from PET scans have been confirmed by Functional MRI (fMRI). The latter looks at the blood flow into different areas of the brain. Using both these techniques, scientists have discovered that depressed people have less activity in the prefrontal cortex, including the ventromedial cortex. Paradoxically, there is more blood flow to the limbic area which contains the hippocampus, despite the shrinkage of the hippocampus in depression.
Electroencephalogram (EEG)
There can be changes in the rapid eye movement (REM) pattern as well as the slow wave phase of the sleep cycle. The EEG shows decreased REM sleep latency, decreased slow wave activity, and deeper delta waves in depressed subjects.
Blood Tests
Blood is taken to exclude hypothyroidism, high cortisol levels, vitamin deficiencies, and if consumption of recreational drugs (e.g. amphetamines) is suspected, blood can be taken to confirm their presence. Patients with high cholesterol levels might be taking statins, a potential cause of depression.
Treatments
Between 70-80% will improve their depressive symptoms if treated correctly. Whether or not antidepressants will lower suicide risk is a controversial topic; epidemiological studies have shown conflicting results, some showing increased and others showing decreased risk of suicide (28).
Antidepressants
a) Selective Serotonin Reuptake Inhibitors (SSRIs) (Citalopram, Escitalopram, Fluoxetine, Sertraline) (11)
This medicine blocks the reuptake of serotonin in the brain’s synaptic gap, and thereby prolongs the amount of serotonin in the synapse, enhancing neurotransmission. Serotonin is associated with happiness. SSRIs are generally preferred over other medicines, especially in children, adolescents, and late-onset depression. Adverse reactions are also less than other antidepressants. They include gastrointestinal upsets, sexual dysfunction, fatigue and restlessness. Citalopram when given in higher doses may cause prolongation of the cardiac QT interval.
In the 1990s, some 3% of American were taking Prozac, an SSRI antidepressant. The prevalence of consuming antidepressants has quadrupled over the following few decades, and there used to be a joke pointing to the United States as a “Prozac Nation”!
b) Serotonin/Noradrenaline Reupdate Inhibitors (SNRIs) (Veniafaxine, Desvenlafaxine, Duloxetine) (12)
For patients who suffer from pain or extreme tiredness, the SRNIs can be considered as a first-line treatment. SRNIs should be used alone because there are some interactions when combined with other antidepressants. Side effects include dizziness, dry mouth, diarrhoea or constipation.
c) Monoamine Oxidase Inhibitors (MAOIs) (Isocarboxacid, Phenelzine, Selegiline) (13)
Monoamine Oxidase Inhibitors prevent the metabolism of the monoamines 5-hydroxytryptamine (5HT) and noradrenaline, which increases the level of these neurotransmitter monoamines. An important side effect is that the risk of a hypertensive crisis. A low tyramine diet is recommended. Other side effects are insomnia, lack of sleep, anxiety, sexual dysfunction and weight gain.
d) Tricyclic Antidepressants (TCI) (Amitriptyline, Amoxapine, Desipramine) (14)
Tricyclic antidepressants block the reuptake of serotonin and noradrenaline in the presynaptic nerves. They were introduced in the 1950s and are currently used as a second line treatment when other antidepressants are ineffective. They elevate one’s mood. Unfortunately side effects are more common with TCIs, and include drowsiness, blurred vision, dry mouth, constipation, urine retention. They have also been used for people with obsessive-compulsive disorder and can help some who suffer panic disorders.
e) N-Methyl-D-aspartate (NMDA) Antagonists (Esketamine) (15)
The NMDA receptor is activated by glutamate and when that happens, a nerve signal is activated. The NMDA receptor antagonist will block the receptor and hence inhibits electrical impulses to pass. The antidepressant effects of the NMDA Receptor Antagonist can be felt relatively quickly, in about 4 hours.
ElectroConvulsive Therapy (ECT) (16)
A small and controlled amount of electric current is passed through the brain while the patient is under general anaesthesia. This induces a brief seizure. It has been around for decades and is used for major depressive patients. It is effective for about 50% of patients,
Deep Brain Stimulation (17)
Quite recently, neurosurgeons have reported successful treatment of several patients’ severe and treatment-resistant depression by implanting a wire with pacemaker-like device right into particular areas of the brain known as the subgenual cingulate region (also known as Brodmann’s area 25), and a part of the middle frontal cortex. The instrument delivers continual electrical stimulation to these brain areas, and this stimulation had a pronounced anti-depressant effect. Exactly why and how this treatment appears to work is unclear. Stimulation of these regions, which connects the limbic (emotion) centres in the brain with the frontal cortex can better manage and regulate one’s emotions. The frontal cortex might then help reduce depressive thoughts. Further research is in the pipeline.
Transcranial Magnetic Stimulation (18)
This is a noninvasive procedure using magnetic fields applied externally to stimulate part of the brain in order to alleviate depression. An electromagnetic coil delivers the magnetic waves to the frontal cortex. It is painless, safe and well-tolerated. The exact mechanism is unknown but it is speculated that the magnetic waves might stimulate that part of the brain which is underactive in people who have depression. Side effects are uncommon, and include headaches, twitching of the facial muscles, lightheadedness, and some tingling sensations. It works in about 30% of depressives, and fails in 50-60% of patients.
Non-Pharmacological Treatments
Psychotherapy (19)
Psychotherapy, or talk therapy, can help alleviate depression, and appears to be better in maintaining longterm alleviation. This includes cognitive behavioural therapy, interpersonal therapy, and psychodynamic therapy. They help the individual to focus on the present, and encourages the regaining of control over mood and function. Success for this type of therapy depends on the relationship between the patient and therapist.
Social Support
Love and support from family and friends helps tremendously. Strong social support leads to better longterm outcomes.
Music and Art Therapy (20,21)
Music and art therapy have both been shown to help people with depression. They make one feel more relaxed, they soothe the mind, and they lift one’s spirits.
Physical Activities (22)

Physical activities help reduce depression. Theories of why it works include the increased release of neurotransmitters, endorphins and endocannabinoids. Also tense muscles are relaxed. Exercising for 20 minutes x3 per week is effective.
Diet (23)
Although the evidence linking diet and relieving depression is not absolutely definitive, it is possible that eating more fruits and vegetables may have some benefits.
Suicide (24,25)

In Singapore, suicide is the leading cause of death for those aged 10-29. In 2020 there were 452 lives lost to suicide, amounting to 5 times more deaths from suicide than transport accidents (1). Males accounted for more than 70% of all suicides in 2020. For every suicide, at least 6 attempted suicide survivors are left behind.
The Risk Factors
Keep a lookout for risk factors. If you hear or observe any of the following, talk to the individual, asking how things are,
- Previous attempt or family history of suicide
- Depression and other mental health problems
- Serious or chronic health conditions, terminal illness
- Distressing life events (failing exams, divorce, job loss, death of close ones, etc.)
- Prolonged stress factors (bullying, cyberbullying, physical and emotional abuse, unemployment, etc.)
- Alcoholic, substance abuse (heroin, amphetamines, etc)
The Warning Signs
Listen Carefully
If you hear someone say anything like the following, take what they say seriously. Do not dismiss it summarily, and do not say “Everything will be all right”. Better to ask “Is there something bothering you?” “Are you unhappy about something?”
- “My family will be better off without me”
- “My life is meaningless anyway”
- “If you don’t love me, I’ll kill myself”
Unusual Actions or Writings
If you see someone doing the following or posting messages on the internet, it is better to err on the side of caution and discuss the matter with that person. “Anything the matter?” “Can we talk about what’s happening?”
- Writing about departing from this world, talking about sadness, suicide notes (posting on social media, blogs, group chats, YouTube, etc)
- Giving away treasured possessions and saying goodbye
- Researching suicide methods, buying rope
Changes in Behaviour
- Emotional outbursts (anger, sadness, irritability, recklessness)
- Loss of interest in previously enjoyed activities
- Humiliation or anxiety
- Withdrawal from social activities
The COVID-19 Pandemic and Depression (26,27)
From January 2020, the COVID-19 infection spread rapidly and engulfed the entire world. It changed all our lives. Millions of people have caught the disease, and already over 4 million people have died. Jobs are lost, affecting one’s income, schools and restaurants are restricted, theatre and music performances curtailed, reduced social mobility and social isolation, virtually no air travel, have all made people feel very lonely, and heightened stress, anxiety, frustrations, and hostility. It is estimated that a third of the population are anxious and depressed. Suicide rates have increased markedly (1,2).
At times like this, family, friends and social organisations need to support one another. Mental health counselling services need to be increased. Governments can help by ensuring COVID-19 is under public health control, encouraging vaccinations, and economically they can supplement lost incomes, reduce rental charges, opening up new jobs and training schemes.
Conclusions
It is important to note that suicide is preventable. Just talking to the depressed person can help alleviate suicidal thoughts and prevent a tragedy. Be neutral and do not be judgemental. Telling the person not to worry or that everything will sort itself out, is probably not going to help. Better to spend time listening to the person’s problems, worries, failures, suffering, and fears. Some individuals want to end their life because they want to terminate an unbearably painful situation, but if they can be shown an alternative solution, they may not embark on such an irreversible act. Sometimes you may have to talk to that person’s relatives or mutual friends to make them aware of the situation. If you feel you are not the right person to help, look for someone else who is more likely to be effective. Try to persuade the depressed person or their relatives to seek psychological or medical or any other appropriate help.
24-Hour Helpline: Samaritans of Singapore 1800 221 4444
Please do not lose hope!
References
1. Ng Keng Gene. Suicides reported in Singapore in 2020 amid Covid-19.
https://www.straitstimes.com/singapore/452-suicides-reported-in-singapore-in-2020-amid-covid-19-highest-since-2012
2. Jerry Choong. On average almost four suicide cases reported to police every day, Malaysia.
https://www.malaymail.com/news/malaysia/2021/06/29/covid-19-on-average-almost-four-suicide-cases-reported-to-police-every-day/1985906
3. Wikipedia. Major depressive disorder.
https://en.wikipedia.org/wiki/Major_depressive_disorder
4. eMedicine. Depression
https://emedicine.medscape.com/article/286759-overview#showall
5. Diagnostic and Statistical Manual 5th edition (DSM-V) Diagnosis of depression.
https://www.psycom.net/depression-definition-dsm-5-diagnostic-criteria/
6. Mayo Clinic. Bipolar disorder
https://www.mayoclinic.org/diseases-conditions/bipolar-disorder/symptoms-causes/syc-20355955
7. MentalHelp. Biology of depression.
https://www.mentalhelp.net/depression/biology-genetics-and-imaging/
8. Wikipedia. Biology of depression.
https://en.wikipedia.org/wiki/Biology_of_depression
9. Shadrina M et al. Genetic factors in major depression disorders.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065213/
10. Mayberg HS et al. Reciprocal Limbic-Cortical Function and Negative Mood: Converging PET Findings in Depression and Normal Sadnesshttps://ajp.psychiatryonline.org/doi/full/10.1176/ajp.156.5.675
11. UK NHS. Overview – Selective serotonin reuptake inhibitors (SSRIs)
https://www.nhs.uk/mental-health/talking-therapies-medicine-treatments/medicines-and-psychiatry/ssri-antidepressants/overview/
12. Medical News Today. What to know about serotonin-norepinephrine reuptake inhibitor (SNRI) drugs
https://www.medicalnewstoday.com/articles/snri#stopping
13. Ankrom S. How MAOIs work and common side effects.
https://www.verywellmind.com/monoamine-oxidase-inhibitors-maois-2584303
14. Ogbru A. Tricyclic antidepressants (TCAs).
https://www.rxlist.com/tricyclic_antidepressants_tcas/drug-class.htm
15. Pochwat B et al. An update on NMDA antagonists in depression
https://pubmed.ncbi.nlm.nih.gov/31328587/
16. American Psychiatric Association. What is ElectroConvulsive Therapy (ECT)?
https://www.psychiatry.org/patients-families/ect
17. ScienceDaily. Long-term study data shows Deep Brain Stimulation (DBS) is effective treatment for most severe form of depression.
https://www.sciencedaily.com/releases/2019/10/191004074901.htm
18. Mayo Clinic. Transcranial magnetic stimulation.
https://www.mayoclinic.org/tests-procedures/transcranial-magnetic-stimulation/about/pac-20384625
19. Cleveland Clinic. Psychotherapy for depression.
https://my.clevelandclinic.org/health/treatments/9300–psychotherapy-for-depression
20. MedicalNewsToday. What is music therapy and how does it work?
https://www.medicalnewstoday.com/articles/music-therapy#for-depression
21. VeryWellMind. What is art therapy?
https://www.verywellmind.com/what-is-art-therapy-2795755
22. Mayo Clinic. Depression and anxiety: exercise eases symptoms.
https://www.mayoclinic.org/diseases-conditions/depression/in-depth/depression-and-exercise/art-20046495
23. MedicalNewsToday. What foods are good for helping depression?
https://www.medicalnewstoday.com/articles/318428#vitamin-d
24. WebMD. Suicide.
https://www.medicinenet.com/suicide/article.htm
25. Suicide.org. How to help.
http://www.suicide.org/how-to-talk-to-suicidal-callers.html
26. US CDC. COVID-19 coping with stress.
https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
27. Duke-NUS. COVID-19: 1 in 3 adults anxious, depressed.
https://www.duke-nus.edu.sg/allnews/covid-19-1-in-3-adults-anxious-depressed
28. Wikipedia. Antidepressants and suicide risk.
https://en.wikipedia.org/wiki/Antidepressants_and_suicide_risk
Getting Help
National Care Hotline: 1800-202-6868 (8am to noon)
Mental Well-Being
Mental Health Helpline: 6389-2222 (24 hours)
Samaritans of Singapore: 1800-221-4444 (24 hours)
Singapore Association for Mental Health: 1800-283-7019 (Mon to Fri 9am to 6pm)
Silver Ribbon Singapore: 6386-1928, 6509-0271 (Mon to Fri 9am to 6pm)
Tinkle Friend: 1800-274-4788 (Mon to Fri 2:30 to 5pm)
Counselling
Touchline 1800-377-2252 (Mon to Fri 9am to 6pm)
Care Corner Counselling Centre (Mandarin): 1800-353-5800 (10am to 10pm)
Written by Kenneth Lyen 13 July 2021
You must be logged in to post a comment.